Sunday Poster Session
Category: Liver
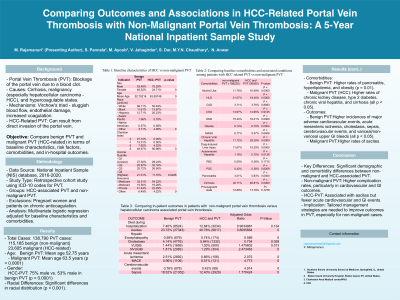
P1249 - Comparing Outcomes and Associations in HCC-Related Portal Vein Thrombosis With Non-Malignant Portal Vein Thrombosis: A 5-Year National Inpatient Sample Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Medha Rajamanuri, MBBS
Southern Illinois University
springfield, IL
Presenting Author(s)
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Mark Ayoub, MD3, Vinay Jahagirdar, MD4, Sophia dar, MD1, Muhammad YN. Chaudhary, MBChB5, Vishwajit Kode, MD6, Nadeem Anwar, MD7
1Southern Illinois University, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3Charleston Area Medical Center, Charleston, WV; 4University of Missouri - Kansas City School of Medicine, Kansas City, MO; 5Indiana University Southwest, Evansville, IN; 6California Pacific Medical Center, San Francisco, CA; 7West Virginia University Charleston Area Medical Center, Charleston, WV
Introduction: Portal vein thrombosis (PVT) is a blockage of the portal vein caused by a blood clot, often due to cirrhosis, malignancy, or other hypercoagulable states involving Virchow's triad: sluggish blood flow, endothelial damage, and increased blood coagulation. In hepatocellular carcinoma (HCC) patients, PVT can also result from direct invasion of the portal vein. This study compares benign PVT and malignant PVT (secondary to HCC) by examining baseline characteristics, risk factors, comorbidities, and in-hospital outcomes.
Methods: Using the National Inpatient Sample (NIS) database from 2016 to 2020, we identified hospitalizations with PVT associated with HCC and non-malignant PVT using ICD-10 codes. This retrospective cohort study excluded pregnant women and patients on chronic anticoagulation. Multivariate logistic regression compared outcomes adjusted for baseline characteristics and comorbidities.
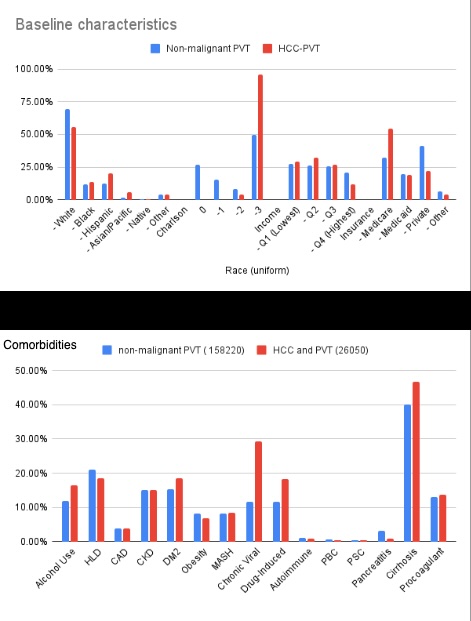
Results: The study investigated 138,790 PVT cases: 115,185 benign and 23,605 malignant. Benign PVT patients had a mean age of 52.75 years, compared to 63.5 years in malignant cases (p < 0.0001). HCC-PVT was more common in males (75% vs. 53%, p < 0.0001), with significant racial differences (p < 0.001). Benign PVT had higher rates of pancreatitis, hyperlipidemia, and obesity (p = 0.01), while malignant PVT was associated with higher rates of chronic kidney disease, type 2 diabetes, chronic viral hepatitis, and cirrhosis (all p < 0.05).
Non-malignant PVT had significantly higher incidences of adverse outcomes, including major adverse cardiovascular events, acute mesenteric ischemia, cholestasis, sepsis, cerebrovascular events, and variceal and non-variceal upper GI bleeds (all p < 0.05).
Discussion: Significant differences exist between non-malignant and HCC-associated PVT in demographics, comorbidities, and in-hospital outcomes. HCC-associated PVT patients have higher rates of ascites, while non-malignant PVT patients face higher rates of complications such as upper GI bleeds, acute mesenteric ischemia, and major cardiovascular and cerebrovascular events. These findings underscore the impact of non-malignant PVT on patient outcomes. Further research is needed to develop tailored management strategies to optimize outcomes for these patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Mark Ayoub, MD3, Vinay Jahagirdar, MD4, Sophia dar, MD1, Muhammad YN. Chaudhary, MBChB5, Vishwajit Kode, MD6, Nadeem Anwar, MD7. P1249 - Comparing Outcomes and Associations in HCC-Related Portal Vein Thrombosis With Non-Malignant Portal Vein Thrombosis: A 5-Year National Inpatient Sample Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Southern Illinois University, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3Charleston Area Medical Center, Charleston, WV; 4University of Missouri - Kansas City School of Medicine, Kansas City, MO; 5Indiana University Southwest, Evansville, IN; 6California Pacific Medical Center, San Francisco, CA; 7West Virginia University Charleston Area Medical Center, Charleston, WV
Introduction: Portal vein thrombosis (PVT) is a blockage of the portal vein caused by a blood clot, often due to cirrhosis, malignancy, or other hypercoagulable states involving Virchow's triad: sluggish blood flow, endothelial damage, and increased blood coagulation. In hepatocellular carcinoma (HCC) patients, PVT can also result from direct invasion of the portal vein. This study compares benign PVT and malignant PVT (secondary to HCC) by examining baseline characteristics, risk factors, comorbidities, and in-hospital outcomes.
Methods: Using the National Inpatient Sample (NIS) database from 2016 to 2020, we identified hospitalizations with PVT associated with HCC and non-malignant PVT using ICD-10 codes. This retrospective cohort study excluded pregnant women and patients on chronic anticoagulation. Multivariate logistic regression compared outcomes adjusted for baseline characteristics and comorbidities.
Results: The study investigated 138,790 PVT cases: 115,185 benign and 23,605 malignant. Benign PVT patients had a mean age of 52.75 years, compared to 63.5 years in malignant cases (p < 0.0001). HCC-PVT was more common in males (75% vs. 53%, p < 0.0001), with significant racial differences (p < 0.001). Benign PVT had higher rates of pancreatitis, hyperlipidemia, and obesity (p = 0.01), while malignant PVT was associated with higher rates of chronic kidney disease, type 2 diabetes, chronic viral hepatitis, and cirrhosis (all p < 0.05).
Non-malignant PVT had significantly higher incidences of adverse outcomes, including major adverse cardiovascular events, acute mesenteric ischemia, cholestasis, sepsis, cerebrovascular events, and variceal and non-variceal upper GI bleeds (all p < 0.05).
Discussion: Significant differences exist between non-malignant and HCC-associated PVT in demographics, comorbidities, and in-hospital outcomes. HCC-associated PVT patients have higher rates of ascites, while non-malignant PVT patients face higher rates of complications such as upper GI bleeds, acute mesenteric ischemia, and major cardiovascular and cerebrovascular events. These findings underscore the impact of non-malignant PVT on patient outcomes. Further research is needed to develop tailored management strategies to optimize outcomes for these patients.
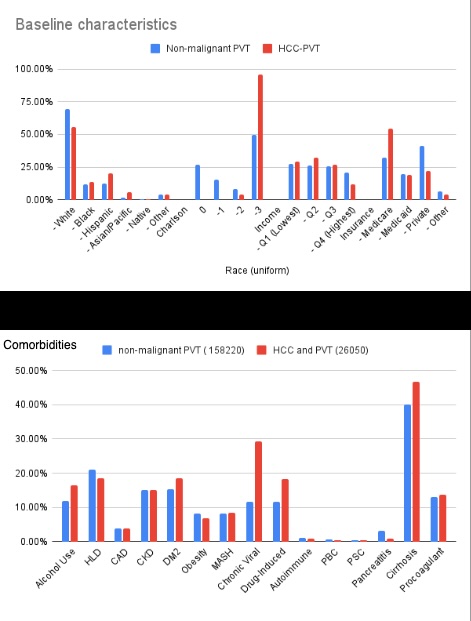
Figure: Baseline characteristics and comorbidities of HCC vs non-malignant PVT
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Medha Rajamanuri indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Mark Ayoub indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Sophia dar indicated no relevant financial relationships.
Muhammad Chaudhary indicated no relevant financial relationships.
Vishwajit Kode indicated no relevant financial relationships.
Nadeem Anwar indicated no relevant financial relationships.
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Mark Ayoub, MD3, Vinay Jahagirdar, MD4, Sophia dar, MD1, Muhammad YN. Chaudhary, MBChB5, Vishwajit Kode, MD6, Nadeem Anwar, MD7. P1249 - Comparing Outcomes and Associations in HCC-Related Portal Vein Thrombosis With Non-Malignant Portal Vein Thrombosis: A 5-Year National Inpatient Sample Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
