Sunday Poster Session
Category: Liver
P1254 - Integration of Palliative Care for Liver Transplant Evaluation in a Tertiary Care Transplant Center - A Quality Improvement Project
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Khushboo V. Bhatia, MBBS
Beth Israel Deaconess Medical Center, Harvard Medical School
Boston, MA
Presenting Author(s)
Khushboo V. Bhatia, MBBS
Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
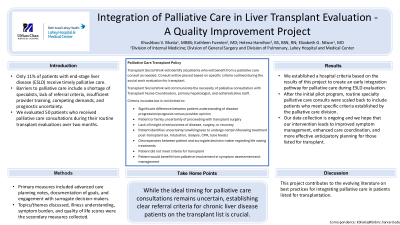
Introduction: Current literature shows underutilization among patients with end-stage liver disease (ESLD) with only 11% of cirrhosis patients receiving specialty palliative care or hospice referrals, often very late. Several barriers to implementing palliative care in liver transplant populations include a shortage of specialized palliative care providers, lack of evidence-based referral criteria, insufficient provider training, competing demands on providers' time, and heterogeneous population and prognostic uncertainty. We describe a quality improvement project at Lahey Hospital and Medical Center that aimed to document the integration of specialty palliative care for patients with ESLD who were routinely evaluated for liver transplantation.
Methods: Our study evaluated the initial cohort of approximately 50 patients who received routine specialty palliative care consult visits by two providers trained in palliative care during their routine outpatient transplant evaluations over two months. The primary measured collected were advanced care planning notes (e.g., MOLST forms, healthcare proxy forms) and the specialty of the provider discussing them, documentation of goals and values, identification and engagement with surrogate decision-makers/healthcare proxy. Topics/themes discussed, illness understanding, symptom burden, and quality of life scores were the secondary measures collected.
Results: After the initial pilot program, routine specialty palliative care consults were scaled back to include patients who meet specific criteria established by the palliative care division. Transplant social work was tasked to identify patients who would benefit from a palliative care consult based on the criteria outlined in Table 1. Our data collection is ongoing and we hope that our intervention leads to improved symptom management, enhanced care coordination, and more effective anticipatory planning.
Discussion: Our goal was to find an optimal pathway for early integration of specialty palliative care services during the transplant evaluation process for ESLD patients. Furthermore, this project will help contribute to the growing body of evidence on best practices to implement specialty palliative care within tertiary care transplant centers.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khushboo V. Bhatia, MBBS. P1254 - Integration of Palliative Care for Liver Transplant Evaluation in a Tertiary Care Transplant Center - A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Current literature shows underutilization among patients with end-stage liver disease (ESLD) with only 11% of cirrhosis patients receiving specialty palliative care or hospice referrals, often very late. Several barriers to implementing palliative care in liver transplant populations include a shortage of specialized palliative care providers, lack of evidence-based referral criteria, insufficient provider training, competing demands on providers' time, and heterogeneous population and prognostic uncertainty. We describe a quality improvement project at Lahey Hospital and Medical Center that aimed to document the integration of specialty palliative care for patients with ESLD who were routinely evaluated for liver transplantation.
Methods: Our study evaluated the initial cohort of approximately 50 patients who received routine specialty palliative care consult visits by two providers trained in palliative care during their routine outpatient transplant evaluations over two months. The primary measured collected were advanced care planning notes (e.g., MOLST forms, healthcare proxy forms) and the specialty of the provider discussing them, documentation of goals and values, identification and engagement with surrogate decision-makers/healthcare proxy. Topics/themes discussed, illness understanding, symptom burden, and quality of life scores were the secondary measures collected.
Results: After the initial pilot program, routine specialty palliative care consults were scaled back to include patients who meet specific criteria established by the palliative care division. Transplant social work was tasked to identify patients who would benefit from a palliative care consult based on the criteria outlined in Table 1. Our data collection is ongoing and we hope that our intervention leads to improved symptom management, enhanced care coordination, and more effective anticipatory planning.
Discussion: Our goal was to find an optimal pathway for early integration of specialty palliative care services during the transplant evaluation process for ESLD patients. Furthermore, this project will help contribute to the growing body of evidence on best practices to implement specialty palliative care within tertiary care transplant centers.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khushboo Bhatia indicated no relevant financial relationships.
Khushboo V. Bhatia, MBBS. P1254 - Integration of Palliative Care for Liver Transplant Evaluation in a Tertiary Care Transplant Center - A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
