Sunday Poster Session
Category: Liver
P1255 - Thrombotic Events in MASLD Cirrhosis Versus Cirrhosis of Other Etiologies: A National Inpatient Sample Population Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Prince A. Ameyaw, MD
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH1, Rofina Johnkennedy, MD, MPH1, Karthik Mathialagan, MD1, Basile Njei, MD2
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale University School of Medicine, New Haven, CT
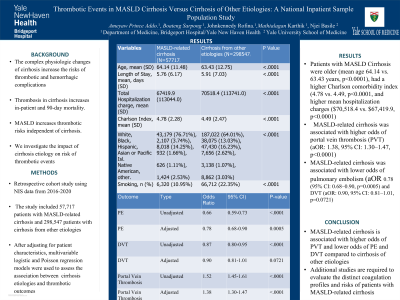
Introduction: The complex homeostatic changes associated with cirrhosis increase the risks of both hemorrhagic and thrombotic complications. Thrombosis in cirrhosis is linked to higher in-patient and 90-day mortality. Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) increases the risk of systemic and portal thrombosis independent of liver cirrhosis. This study evaluates thrombotic risks in patients with MASLD-related cirrhosis compared to those with cirrhosis of other etiologies.
Methods: We conducted a retrospective analysis using the National Inpatient Sample (NIS) database from 2016 to 2020, identifying patients diagnosed with cirrhosis due to MASLD and other causes. Patient characteristics, comorbidities, and outcomes were compared between these groups. After adjusting for age, sex, race, smoking, cardiometabolic risk factors, hospital characteristics, admission type, year of admission, socio-economic factors, and baseline comorbidities, multivariable logistic and Poisson regression models assessed the association between MASLD-related cirrhosis and thrombotic outcomes.
Results: The study included 57,717 patients with MASLD-related cirrhosis and 298,547 patients with cirrhosis from other etiologies. Patients with MASLD-related cirrhosis were older (mean age 64.14 vs. 63.43 years, p< 0.0001), had higher mean hospitalization charges ($70,518.4 vs. $67,419.9, p< 0.0001), and a higher Charlson Comorbidity Index (4.78 vs. 4.49, p< 0.0001). Thrombotic events differed significantly between the two groups. For MASLD-related cirrhosis, the adjusted odds ratio (aOR) for pulmonary embolism (PE) was 0.78 (95% CI: 0.68–0.90, p=0.0005) and for deep vein thrombosis (DVT) was 0.90 (95% CI: 0.81–1.01, p=0.0721), indicating lower risks compared to other cirrhosis etiologies. Conversely, MASLD-related cirrhosis was associated with higher adjusted odds of portal vein thrombosis (PVT) (aOR: 1.38, 95% CI: 1.30–1.47, p< 0.0001) and superficial venous thrombosis (SVT) (aOR: 1.29, 95% CI: 1.22–1.37, p< 0.0001).
Discussion: The etiology of cirrhosis impacts the development of systemic and portal vein thrombotic events. Patients with MASLD-related cirrhosis had a reduced risk of developing venous thromboembolism (VTE) but were more likely to develop PVT and SVT compared to other etiologies. As the prevalence of MASLD-related cirrhosis continues to rise, further studies are needed to understand its distinct thrombotic risks to improve management and clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH1, Rofina Johnkennedy, MD, MPH1, Karthik Mathialagan, MD1, Basile Njei, MD2. P1255 - Thrombotic Events in MASLD Cirrhosis Versus Cirrhosis of Other Etiologies: A National Inpatient Sample Population Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale University School of Medicine, New Haven, CT
Introduction: The complex homeostatic changes associated with cirrhosis increase the risks of both hemorrhagic and thrombotic complications. Thrombosis in cirrhosis is linked to higher in-patient and 90-day mortality. Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) increases the risk of systemic and portal thrombosis independent of liver cirrhosis. This study evaluates thrombotic risks in patients with MASLD-related cirrhosis compared to those with cirrhosis of other etiologies.
Methods: We conducted a retrospective analysis using the National Inpatient Sample (NIS) database from 2016 to 2020, identifying patients diagnosed with cirrhosis due to MASLD and other causes. Patient characteristics, comorbidities, and outcomes were compared between these groups. After adjusting for age, sex, race, smoking, cardiometabolic risk factors, hospital characteristics, admission type, year of admission, socio-economic factors, and baseline comorbidities, multivariable logistic and Poisson regression models assessed the association between MASLD-related cirrhosis and thrombotic outcomes.
Results: The study included 57,717 patients with MASLD-related cirrhosis and 298,547 patients with cirrhosis from other etiologies. Patients with MASLD-related cirrhosis were older (mean age 64.14 vs. 63.43 years, p< 0.0001), had higher mean hospitalization charges ($70,518.4 vs. $67,419.9, p< 0.0001), and a higher Charlson Comorbidity Index (4.78 vs. 4.49, p< 0.0001). Thrombotic events differed significantly between the two groups. For MASLD-related cirrhosis, the adjusted odds ratio (aOR) for pulmonary embolism (PE) was 0.78 (95% CI: 0.68–0.90, p=0.0005) and for deep vein thrombosis (DVT) was 0.90 (95% CI: 0.81–1.01, p=0.0721), indicating lower risks compared to other cirrhosis etiologies. Conversely, MASLD-related cirrhosis was associated with higher adjusted odds of portal vein thrombosis (PVT) (aOR: 1.38, 95% CI: 1.30–1.47, p< 0.0001) and superficial venous thrombosis (SVT) (aOR: 1.29, 95% CI: 1.22–1.37, p< 0.0001).
Discussion: The etiology of cirrhosis impacts the development of systemic and portal vein thrombotic events. Patients with MASLD-related cirrhosis had a reduced risk of developing venous thromboembolism (VTE) but were more likely to develop PVT and SVT compared to other etiologies. As the prevalence of MASLD-related cirrhosis continues to rise, further studies are needed to understand its distinct thrombotic risks to improve management and clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prince Ameyaw indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Rofina Johnkennedy indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH1, Rofina Johnkennedy, MD, MPH1, Karthik Mathialagan, MD1, Basile Njei, MD2. P1255 - Thrombotic Events in MASLD Cirrhosis Versus Cirrhosis of Other Etiologies: A National Inpatient Sample Population Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
