Sunday Poster Session
Category: Liver
P1259 - Sarcopenia and Pre- and Post-Liver Transplantation Mortality in Cirrhosis From Metabolic Dysfunction- Associated Steatotic Liver Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- GH
Gregory Habig, MD
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Gregory Habig, MD1, Justin Bilello, MD1, Christa Smaltz, MD2, Shahir Monsuruddin, MD1, Flavius Guglielmo, MD1, Ethan Halpern, MD1, Dina Halegoua-DeMarzio, MD1
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Metabolic-dysfunction associated steatotic liver disease (MASLD) is an increasing cause of cirrhosis and liver transplantation worldwide. One factor associated with poor outcomes post liver transplantation (LT) is sarcopenia. This study aims to describe LT outcomes in patients with MASLD cirrhosis by evaluating pre and post-LT mortality in patients with and without sarcopenia.
Methods: Computed tomography (CT) or magnetic resonance (MR) imaging were obtained in 406 cases of MASLD diagnosed by liver biopsy at a single transplant center. 175 cases were included based on imaging availability within 18 months of biopsy demonstrating cirrhosis. Cases with biopsy evidence of another cause of cirrhosis, presence of malignancy, or radiologic factors affecting psoas measurement were excluded. Sarcopenia was defined by psoas muscle area (PMA) of < 1561 mm2 in men and < 1464 mm2 in women and psoas muscle index (PMI) of < 5.1 cm2/m2 in men and < 4.3 cm2/m2 in women measured at the L3 level on CT or MR. 6-month pre-LT mortality was assessed at 6-months after image acquisition. Post-LT survival was assessed at 6 months and 1-year after LT. Statistical analysis included chi squared comparing sarcopenia and pre and post-LT survival.
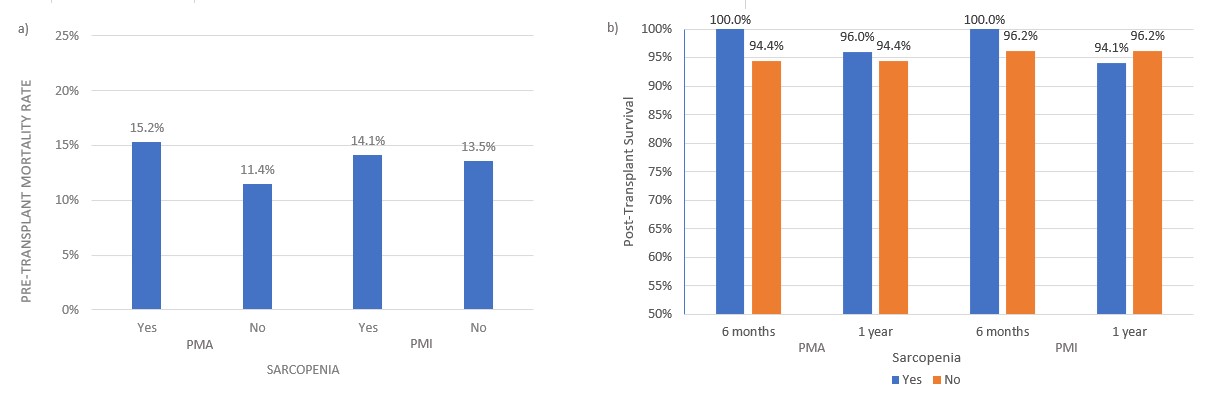
Results: Defined by PMA, 16/105 (15.2%) patients with sarcopenia died within 6 months of imaging compared to 8/70 (11.4%) without sarcopenia (p=0. 0.473). By PMI, 9/64 (14.1%) patients with sarcopenia died within 6 months of imaging compared to 15/111 (13.5%) without sarcopenia (p= 0.919). 43/175 cases underwent LT. 25 patients with sarcopenia by PMA underwent LT. 100% were alive at 6 months and 24/25 (96.0%) at 1 year. 18 patients without sarcopenia by PMA underwent LT, 17/18 were alive at 6 months and 1 year (94.4%) (6-month p= 0.233; 1 year p= 0.811). 17 patients with sarcopenia by PMI underwent LT. 100% were alive at 6 months and 16/17 (94.1%) at 1 year. 26 patients without sarcopenia by PMI underwent LT. 25/26 were alive at 6 months and 1 year (96.2%) (6-month p= 0.413; 1 year p= 0.757) (Fig. 1).
Discussion: Patients with sarcopenia by PMA and PMI showed higher rates of 6-month pre-LT mortality, but this trend failed to reach statistical significance. 6 month and 1 year post-LT survival was high irrespective of sarcopenia presence. Further investigation is needed to determine if the observed trends hold and if sarcopenia based on PMA or PMI could be used as a predictor of pre- and post-LT mortality in MASLD.
Disclosures:
Gregory Habig, MD1, Justin Bilello, MD1, Christa Smaltz, MD2, Shahir Monsuruddin, MD1, Flavius Guglielmo, MD1, Ethan Halpern, MD1, Dina Halegoua-DeMarzio, MD1. P1259 - Sarcopenia and Pre- and Post-Liver Transplantation Mortality in Cirrhosis From Metabolic Dysfunction- Associated Steatotic Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Metabolic-dysfunction associated steatotic liver disease (MASLD) is an increasing cause of cirrhosis and liver transplantation worldwide. One factor associated with poor outcomes post liver transplantation (LT) is sarcopenia. This study aims to describe LT outcomes in patients with MASLD cirrhosis by evaluating pre and post-LT mortality in patients with and without sarcopenia.
Methods: Computed tomography (CT) or magnetic resonance (MR) imaging were obtained in 406 cases of MASLD diagnosed by liver biopsy at a single transplant center. 175 cases were included based on imaging availability within 18 months of biopsy demonstrating cirrhosis. Cases with biopsy evidence of another cause of cirrhosis, presence of malignancy, or radiologic factors affecting psoas measurement were excluded. Sarcopenia was defined by psoas muscle area (PMA) of < 1561 mm2 in men and < 1464 mm2 in women and psoas muscle index (PMI) of < 5.1 cm2/m2 in men and < 4.3 cm2/m2 in women measured at the L3 level on CT or MR. 6-month pre-LT mortality was assessed at 6-months after image acquisition. Post-LT survival was assessed at 6 months and 1-year after LT. Statistical analysis included chi squared comparing sarcopenia and pre and post-LT survival.
Results: Defined by PMA, 16/105 (15.2%) patients with sarcopenia died within 6 months of imaging compared to 8/70 (11.4%) without sarcopenia (p=0. 0.473). By PMI, 9/64 (14.1%) patients with sarcopenia died within 6 months of imaging compared to 15/111 (13.5%) without sarcopenia (p= 0.919). 43/175 cases underwent LT. 25 patients with sarcopenia by PMA underwent LT. 100% were alive at 6 months and 24/25 (96.0%) at 1 year. 18 patients without sarcopenia by PMA underwent LT, 17/18 were alive at 6 months and 1 year (94.4%) (6-month p= 0.233; 1 year p= 0.811). 17 patients with sarcopenia by PMI underwent LT. 100% were alive at 6 months and 16/17 (94.1%) at 1 year. 26 patients without sarcopenia by PMI underwent LT. 25/26 were alive at 6 months and 1 year (96.2%) (6-month p= 0.413; 1 year p= 0.757) (Fig. 1).
Discussion: Patients with sarcopenia by PMA and PMI showed higher rates of 6-month pre-LT mortality, but this trend failed to reach statistical significance. 6 month and 1 year post-LT survival was high irrespective of sarcopenia presence. Further investigation is needed to determine if the observed trends hold and if sarcopenia based on PMA or PMI could be used as a predictor of pre- and post-LT mortality in MASLD.
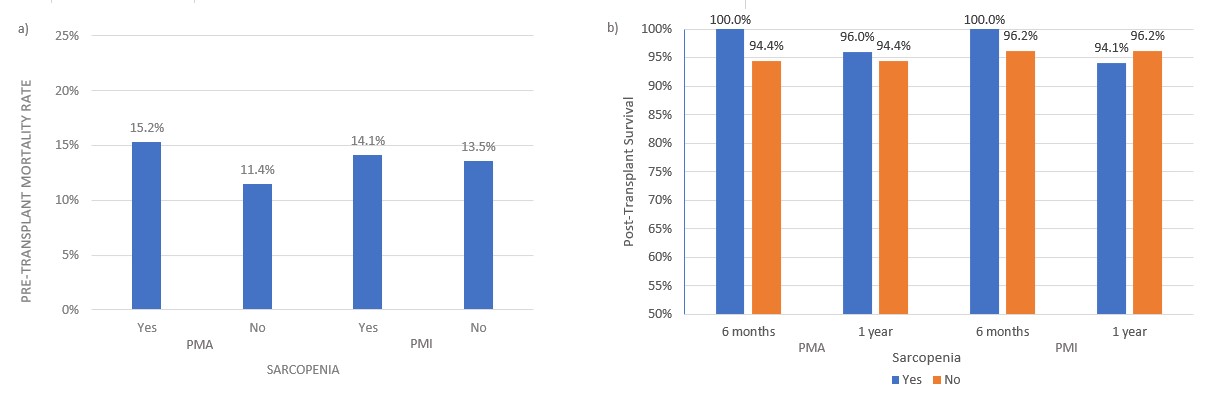
Figure: a) 6-month pre-transplant mortality data showing 16/105 (15.2%) patients with sarcopenia died within 6 months of imaging compared to 8/70 (11.4%) without sarcopenia by PMA (p=0.236). When defined by PMI, 9/64 (14.1%) patients with sarcopenia died within 6 months of imaging compared to 15/111 (13.5%) without sarcopenia. (p=0.460). b) 6-month and 1-year post-transplant survival data demonstrating 25/25 (100%) survival at 6 months and 24/25 (96.0%) alive at 1 year in patients with sarcopenia by PMA compared to 17/18 alive at 6 months and one year (94.4%) in those without sarcopenia (p= 0.233; p= 0.811). When defined by PMI, there were 17/17 (100%) alive at 6 months and 16/17 (94.1%) at 1 year in those with sarcopenia compared 25/26 alive at 6 months and 1 year (96.2%) in those without sarcopenia (p= 0.413; p= 0.757).
Disclosures:
Gregory Habig indicated no relevant financial relationships.
Justin Bilello indicated no relevant financial relationships.
Christa Smaltz indicated no relevant financial relationships.
Shahir Monsuruddin indicated no relevant financial relationships.
Flavius Guglielmo indicated no relevant financial relationships.
Ethan Halpern indicated no relevant financial relationships.
Dina Halegoua-DeMarzio: Akero – Grant/Research Support. Galectin – Grant/Research Support. Madigral – Advisor or Review Panel Member, Grant/Research Support. Novo Nordisk – Advisory Committee/Board Member, Grant/Research Support. Viking – Grant/Research Support.
Gregory Habig, MD1, Justin Bilello, MD1, Christa Smaltz, MD2, Shahir Monsuruddin, MD1, Flavius Guglielmo, MD1, Ethan Halpern, MD1, Dina Halegoua-DeMarzio, MD1. P1259 - Sarcopenia and Pre- and Post-Liver Transplantation Mortality in Cirrhosis From Metabolic Dysfunction- Associated Steatotic Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
