Sunday Poster Session
Category: Liver
P1262 - Taking it to Heart: Hypothyroid Hepatopathy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Marisa-Nicole Zayat, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Marisa-Nicole Zayat, MD1, Micah Vander Griend, MPH1, Bassem Matta, MD2, Cameron Frederick, MD3, Tessa Rohrberg, MD1, Maryam Dalili, MD3, Sunyoung Yoon, MD3, Lynn Fisher, MD1, Estephan Zayat, MD2
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS; 3Wesley Family Medicine Residency, Wichita, KS
Introduction: The majority of pericardial effusions are idiopathic, likely due to infections. Noninfectious causes include autoimmune conditions, neoplasms, drugs, and rarely hypothyroidism.
Case Description/Methods: A 47-year-old female was admitted for recurrent syncope without chest pain, dyspnea, or prodrome. She endorsed progressive exertional and paroxysmal nocturnal dyspnea, chronic cough with blood-tinged sputum, poor appetite, weight loss, fatigue, weakness, pedal edema, orthopnea, and numbness causing unstable gait. She denied fever, chills, chest pain, abdominal pain, nausea, vomiting, diarrhea, or recent sick contacts.
Pre-admission echocardiogram two-weeks prior showed an ejection fraction of 20-25%, moderate mitral and tricuspid regurgitation, left ventricular hypertrophy, enlarged left atrium, inferior vena cava dilation, and pericardial effusion.
On admission her vitals were normal. She was found to be profoundly hypothyroid, with a free T4 of < 0.1 ng/dL and TSH of 61 uIU/mL. Hepatotoxic medications were held for elevated LFTs (Table 1). BNP, D-Dimer, and troponin were elevated. CTA was negative for a pulmonary embolism but revealed cardiomegaly with an enlarging pericardial effusion. No infectious cause was identified. The patient denied a history of autoimmune conditions or neoplasms. No trauma or drugs were implicated.
The patient was monitored via continuous telemetry. IV thyroxine, furosemide, enalapril, metoprolol, and fluid restriction were started. Her TSH gradually improved. Due to the effusion’s chronicity and lack of clinical tamponade, pericardiocentesis was deferred.
On hospital day 9, gastroenterology was consulted for elevated LFTs (Table 2), PT, and INR. She never experienced hypotension during her admission. Extensive acute hepatitis workup was negative. CT and ultrasound showed hepatomegaly with hepatic steatosis, focal fatty sparing, small perihepatic ascites, scattered intraperitoneal fat stranding, and diffuse body wall edema consistent with CHF. Aggressive diuresis with furosemide and spironolactone along with lactulose and UDCA were continued. With treatment, her LFTs trended down, with continued improvement five weeks post-discharge.
Discussion: Hypothyroidism is an uncommon cause of pericardial effusions, reported in 0-10% of cases. Given the acute increase in LFTs and Doppler evidence of CHF, congestive hepatopathy was diagnosed. This case highlights the need for further research on early aggressive intervention in treating hypothyroid-related hepatopathy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Marisa-Nicole Zayat, MD1, Micah Vander Griend, MPH1, Bassem Matta, MD2, Cameron Frederick, MD3, Tessa Rohrberg, MD1, Maryam Dalili, MD3, Sunyoung Yoon, MD3, Lynn Fisher, MD1, Estephan Zayat, MD2. P1262 - Taking it to Heart: Hypothyroid Hepatopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS; 3Wesley Family Medicine Residency, Wichita, KS
Introduction: The majority of pericardial effusions are idiopathic, likely due to infections. Noninfectious causes include autoimmune conditions, neoplasms, drugs, and rarely hypothyroidism.
Case Description/Methods: A 47-year-old female was admitted for recurrent syncope without chest pain, dyspnea, or prodrome. She endorsed progressive exertional and paroxysmal nocturnal dyspnea, chronic cough with blood-tinged sputum, poor appetite, weight loss, fatigue, weakness, pedal edema, orthopnea, and numbness causing unstable gait. She denied fever, chills, chest pain, abdominal pain, nausea, vomiting, diarrhea, or recent sick contacts.
Pre-admission echocardiogram two-weeks prior showed an ejection fraction of 20-25%, moderate mitral and tricuspid regurgitation, left ventricular hypertrophy, enlarged left atrium, inferior vena cava dilation, and pericardial effusion.
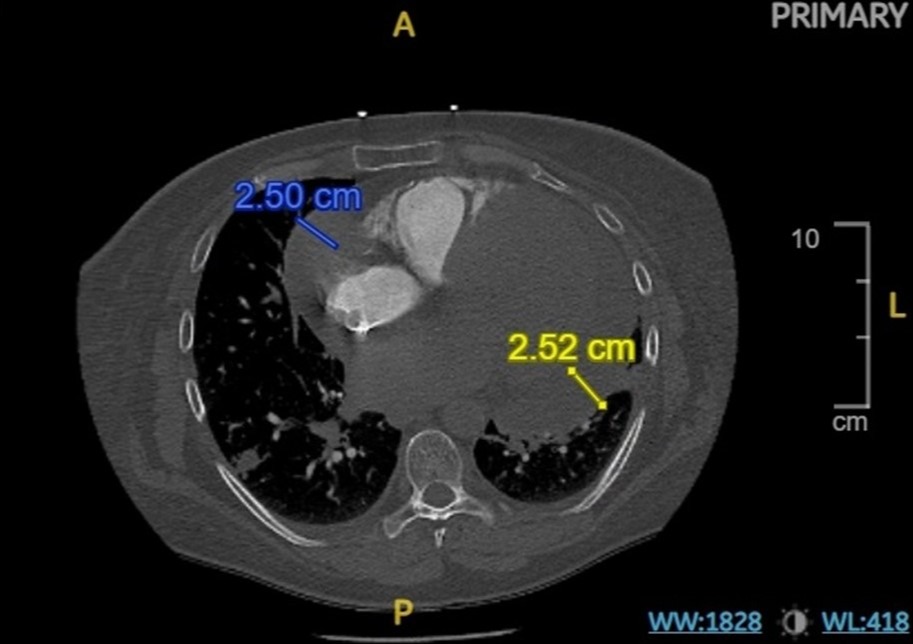
On admission her vitals were normal. She was found to be profoundly hypothyroid, with a free T4 of < 0.1 ng/dL and TSH of 61 uIU/mL. Hepatotoxic medications were held for elevated LFTs (Table 1). BNP, D-Dimer, and troponin were elevated. CTA was negative for a pulmonary embolism but revealed cardiomegaly with an enlarging pericardial effusion. No infectious cause was identified. The patient denied a history of autoimmune conditions or neoplasms. No trauma or drugs were implicated.
The patient was monitored via continuous telemetry. IV thyroxine, furosemide, enalapril, metoprolol, and fluid restriction were started. Her TSH gradually improved. Due to the effusion’s chronicity and lack of clinical tamponade, pericardiocentesis was deferred.
On hospital day 9, gastroenterology was consulted for elevated LFTs (Table 2), PT, and INR. She never experienced hypotension during her admission. Extensive acute hepatitis workup was negative. CT and ultrasound showed hepatomegaly with hepatic steatosis, focal fatty sparing, small perihepatic ascites, scattered intraperitoneal fat stranding, and diffuse body wall edema consistent with CHF. Aggressive diuresis with furosemide and spironolactone along with lactulose and UDCA were continued. With treatment, her LFTs trended down, with continued improvement five weeks post-discharge.
Discussion: Hypothyroidism is an uncommon cause of pericardial effusions, reported in 0-10% of cases. Given the acute increase in LFTs and Doppler evidence of CHF, congestive hepatopathy was diagnosed. This case highlights the need for further research on early aggressive intervention in treating hypothyroid-related hepatopathy.
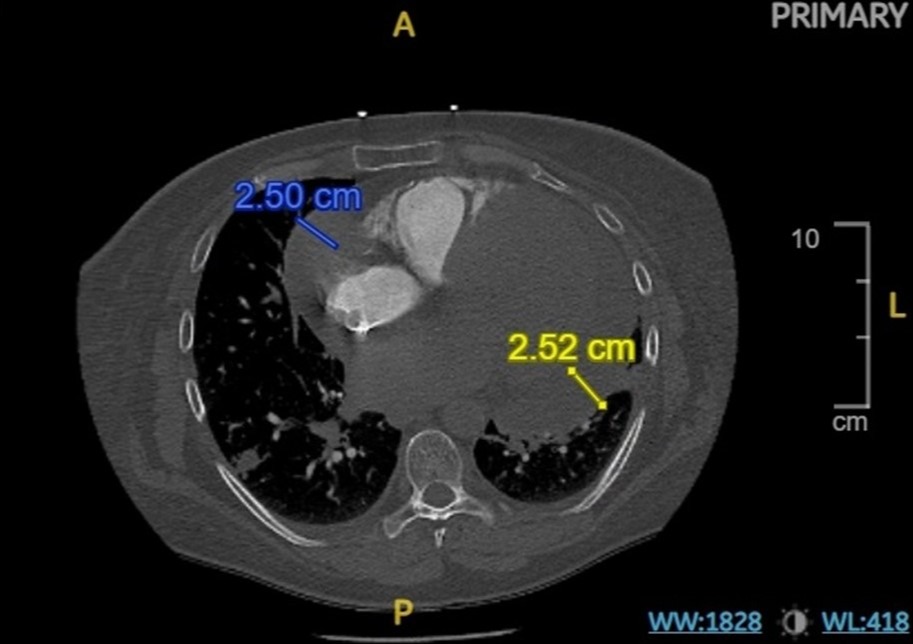
Figure: Figure 1. Axial CT depicts a large pericardial effusion.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Marisa-Nicole Zayat indicated no relevant financial relationships.
Micah Vander Griend indicated no relevant financial relationships.
Bassem Matta indicated no relevant financial relationships.
Cameron Frederick indicated no relevant financial relationships.
Tessa Rohrberg indicated no relevant financial relationships.
Maryam Dalili indicated no relevant financial relationships.
Sunyoung Yoon indicated no relevant financial relationships.
Lynn Fisher indicated no relevant financial relationships.
Estephan Zayat indicated no relevant financial relationships.
Marisa-Nicole Zayat, MD1, Micah Vander Griend, MPH1, Bassem Matta, MD2, Cameron Frederick, MD3, Tessa Rohrberg, MD1, Maryam Dalili, MD3, Sunyoung Yoon, MD3, Lynn Fisher, MD1, Estephan Zayat, MD2. P1262 - Taking it to Heart: Hypothyroid Hepatopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
