Sunday Poster Session
Category: Liver
P1265 - A Rare Case of Postpartum Acute Fatty Liver of Pregnancy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AD
Anshuman Desai, MBBS
Ochsner Health Clinic Foundation
New Orleans, LA
Presenting Author(s)
Anshuman Desai, MBBS, Jasmine McNair, MD, Ruona Ebiai, MD, Natalie Bzowej, MD
Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Acute fatty liver of pregnancy (AFLP) is a rare obstetric emergency characterized by maternal liver dysfunction or failure. It generally occurs in the third trimester and treatment is prompt delivery. Postpartum AFLP is extremely rare with only few case reports available.
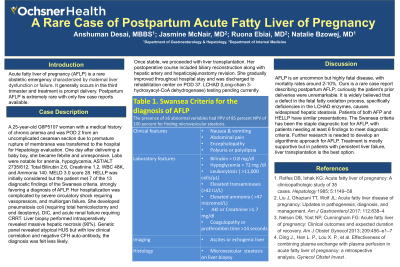
Case Description/Methods: A 25-year-old G6P5107 woman with a medical history of chronic anemia and was POD 2 from an uncomplicated cesarean section due to PROM was transferred to the hospital for Hepatology evaluation. One day after delivering a baby boy, she became febrile and unresponsive. Labs were notable for anemia, hypoglycemia, AST/ALT 2735/612, Total Bilirubin 2.6, Bicarbonate < 5, Potassium 6.1, Creatinine 1.2, WBC 48K, and Ammonia 140. MELD 3.0 score 28. HELLP was initially considered but the patient met 7 of the 13 diagnostic findings of the Swansea criteria, strongly favoring a diagnosis of AFLP. Her hospitalization was complicated by severe circulatory shock requiring vasopressors, and multiorgan failure. She developed pneumatosis coli (requiring total hemicolectomy and end ileostomy), DIC, and right sided hydronephrosis (s/p ureteral stent placement) with acute renal failure requiring CRRT. Liver biopsy performed intraoperatively revealed massive hepatic necrosis (90%). Genetic panel revealed atypical HUS but with low clinical correlation and negative CFH auto-antibody, the diagnosis was less likely.
Once stable, we proceeded with liver transplantation. Her postoperative course included biliary reconstruction along with hepatic artery and hepaticojejunostomy revision. She gradually improved throughout hospital stay and was discharged to rehabilitation center on POD 37. LCHAD (Long-chain 3-hydroxyacyl-CoA dehydrogenase) testing pending currently.
Discussion: AFLP is an uncommon but highly fatal disease, with mortality rates around 2-10%. Ours is a rare case report describing postpartum AFLP; curiously the patient's prior deliveries were unremarkable. It is widely believed that a defect in the fetal fatty oxidation process, specifically deficiencies in the LCHAD enzymes, causes widespread hepatic steatosis. Patients of both AFP and HELLP have similar presentations. The Swansea criteria has been the staple diagnostic tool for AFLP, with patients needing at least 6 findings to meet diagnostic criteria. Further research is needed to develop an algorithmic approach for AFLP. Treatment is mostly supportive but in patients with persistent liver failure, liver transplantation is the best option.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anshuman Desai, MBBS, Jasmine McNair, MD, Ruona Ebiai, MD, Natalie Bzowej, MD. P1265 - A Rare Case of Postpartum Acute Fatty Liver of Pregnancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Acute fatty liver of pregnancy (AFLP) is a rare obstetric emergency characterized by maternal liver dysfunction or failure. It generally occurs in the third trimester and treatment is prompt delivery. Postpartum AFLP is extremely rare with only few case reports available.
Case Description/Methods: A 25-year-old G6P5107 woman with a medical history of chronic anemia and was POD 2 from an uncomplicated cesarean section due to PROM was transferred to the hospital for Hepatology evaluation. One day after delivering a baby boy, she became febrile and unresponsive. Labs were notable for anemia, hypoglycemia, AST/ALT 2735/612, Total Bilirubin 2.6, Bicarbonate < 5, Potassium 6.1, Creatinine 1.2, WBC 48K, and Ammonia 140. MELD 3.0 score 28. HELLP was initially considered but the patient met 7 of the 13 diagnostic findings of the Swansea criteria, strongly favoring a diagnosis of AFLP. Her hospitalization was complicated by severe circulatory shock requiring vasopressors, and multiorgan failure. She developed pneumatosis coli (requiring total hemicolectomy and end ileostomy), DIC, and right sided hydronephrosis (s/p ureteral stent placement) with acute renal failure requiring CRRT. Liver biopsy performed intraoperatively revealed massive hepatic necrosis (90%). Genetic panel revealed atypical HUS but with low clinical correlation and negative CFH auto-antibody, the diagnosis was less likely.
Once stable, we proceeded with liver transplantation. Her postoperative course included biliary reconstruction along with hepatic artery and hepaticojejunostomy revision. She gradually improved throughout hospital stay and was discharged to rehabilitation center on POD 37. LCHAD (Long-chain 3-hydroxyacyl-CoA dehydrogenase) testing pending currently.
Discussion: AFLP is an uncommon but highly fatal disease, with mortality rates around 2-10%. Ours is a rare case report describing postpartum AFLP; curiously the patient's prior deliveries were unremarkable. It is widely believed that a defect in the fetal fatty oxidation process, specifically deficiencies in the LCHAD enzymes, causes widespread hepatic steatosis. Patients of both AFP and HELLP have similar presentations. The Swansea criteria has been the staple diagnostic tool for AFLP, with patients needing at least 6 findings to meet diagnostic criteria. Further research is needed to develop an algorithmic approach for AFLP. Treatment is mostly supportive but in patients with persistent liver failure, liver transplantation is the best option.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anshuman Desai indicated no relevant financial relationships.
Jasmine McNair indicated no relevant financial relationships.
Ruona Ebiai indicated no relevant financial relationships.
Natalie Bzowej indicated no relevant financial relationships.
Anshuman Desai, MBBS, Jasmine McNair, MD, Ruona Ebiai, MD, Natalie Bzowej, MD. P1265 - A Rare Case of Postpartum Acute Fatty Liver of Pregnancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
