Sunday Poster Session
Category: Liver
P1267 - Isolated Polycystic Liver Disease Requiring Transplant- A Rare Indication for MELD Exception
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Zachary C. Vinton, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Award: Presidential Poster Award
Zachary C. Vinton, DO1, Stephanie J. Melquist, MD, MPH2, Clark C. Kulig, MD3
1University of Nebraska Medical Center, Omaha, NE; 2University of Kansas School of Medicine, Wichita, KS; 3Presbyterian St. Luke's Medical Center, Denver, CO
Introduction: Polycystic liver disease (PLD) is a rare genetic disease occurring in isolation in less than 0.01% of cases. Complications can include portal hypertension, liver failure, malnutrition and may require liver transplant. Patients often have preserved synthetic function and low MELD scores, which can limit access to organ transplant without application for MELD exception points. We present a case of isolated PLD with malnutrition and decreasing synthetic function with a request for MELD exception points for transplant candidacy.
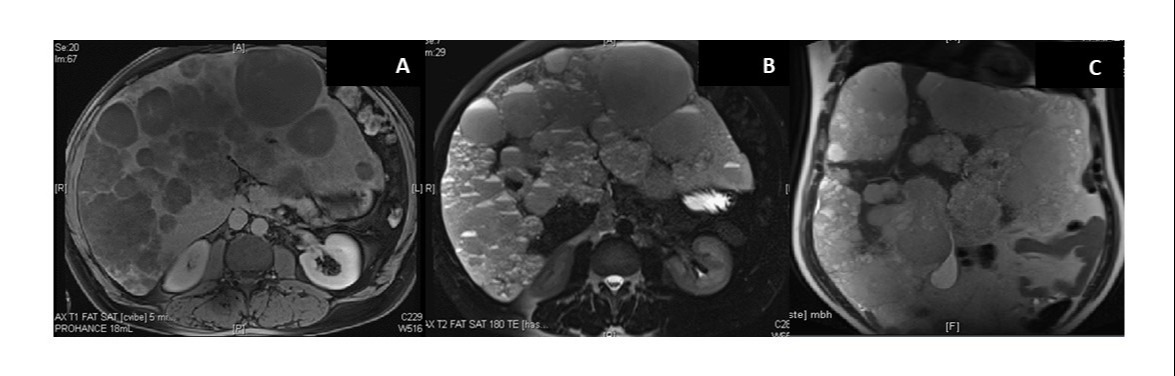
Case Description/Methods: The patient is a 39-year-old male who presented with 30lbs of weight loss over the past year with six months of worsening abdominal pain, distension, early satiety, and anorexia. He has a history of multiple hepatic hemangiomas with no intervention, remote intravenous drug abuse, and no alcohol or tobacco for the past six years. His father died from liver cancer associated with hepatitis C. On physical exam, the patient was alert and oriented without scleral icterus or jaundice. His abdomen was soft and non-tender but had tremendous hepatomegaly. No ascites or lower extremity edema were present. Lab values showed reduced platelets with elevated alkaline phosphatase and total bilirubin, leading to a MELD 3.0 of 13 (Table 1).An abdominal MRI showed marked hepatomegaly with innumerable hepatic lesions with fluid-fluid levels. There was severe narrowing of the left portal vein and the middle and left hepatic veins with normal appearing pancreas and kidneys (Figure 1).A diagnosis of PLD was made radiographically using Reynold’s Criteria. Due to widespread cysts throughout hepatic parenchyma, and no surgical treatment options including fenestration, the patient was evaluated for liver transplant with a request for MELD exception points.
Discussion: Although many patients with PLD are asymptomatic with preserved liver function, massive hepatomegaly and cyst burden may lead to complications. Thus, in severely symptomatic patients who cannot undergo or who fail fenestration or resection, a liver transplant may be necessary. Previously, MELD exception points were not granted for isolated PLD; a guideline change in 2022 made these patients eligible to apply. Our patient initially had a MELD of 13, but due to his severe symptoms, reduction in quality of life, moderate malnutrition, and the potential for clinical deterioration, he was deemed to be an excellent candidate for liver transplant. He is currently awaiting MELD exception.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zachary C. Vinton, DO1, Stephanie J. Melquist, MD, MPH2, Clark C. Kulig, MD3. P1267 - Isolated Polycystic Liver Disease Requiring Transplant- A Rare Indication for MELD Exception, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Zachary C. Vinton, DO1, Stephanie J. Melquist, MD, MPH2, Clark C. Kulig, MD3
1University of Nebraska Medical Center, Omaha, NE; 2University of Kansas School of Medicine, Wichita, KS; 3Presbyterian St. Luke's Medical Center, Denver, CO
Introduction: Polycystic liver disease (PLD) is a rare genetic disease occurring in isolation in less than 0.01% of cases. Complications can include portal hypertension, liver failure, malnutrition and may require liver transplant. Patients often have preserved synthetic function and low MELD scores, which can limit access to organ transplant without application for MELD exception points. We present a case of isolated PLD with malnutrition and decreasing synthetic function with a request for MELD exception points for transplant candidacy.
Case Description/Methods: The patient is a 39-year-old male who presented with 30lbs of weight loss over the past year with six months of worsening abdominal pain, distension, early satiety, and anorexia. He has a history of multiple hepatic hemangiomas with no intervention, remote intravenous drug abuse, and no alcohol or tobacco for the past six years. His father died from liver cancer associated with hepatitis C. On physical exam, the patient was alert and oriented without scleral icterus or jaundice. His abdomen was soft and non-tender but had tremendous hepatomegaly. No ascites or lower extremity edema were present. Lab values showed reduced platelets with elevated alkaline phosphatase and total bilirubin, leading to a MELD 3.0 of 13 (Table 1).An abdominal MRI showed marked hepatomegaly with innumerable hepatic lesions with fluid-fluid levels. There was severe narrowing of the left portal vein and the middle and left hepatic veins with normal appearing pancreas and kidneys (Figure 1).A diagnosis of PLD was made radiographically using Reynold’s Criteria. Due to widespread cysts throughout hepatic parenchyma, and no surgical treatment options including fenestration, the patient was evaluated for liver transplant with a request for MELD exception points.
Discussion: Although many patients with PLD are asymptomatic with preserved liver function, massive hepatomegaly and cyst burden may lead to complications. Thus, in severely symptomatic patients who cannot undergo or who fail fenestration or resection, a liver transplant may be necessary. Previously, MELD exception points were not granted for isolated PLD; a guideline change in 2022 made these patients eligible to apply. Our patient initially had a MELD of 13, but due to his severe symptoms, reduction in quality of life, moderate malnutrition, and the potential for clinical deterioration, he was deemed to be an excellent candidate for liver transplant. He is currently awaiting MELD exception.
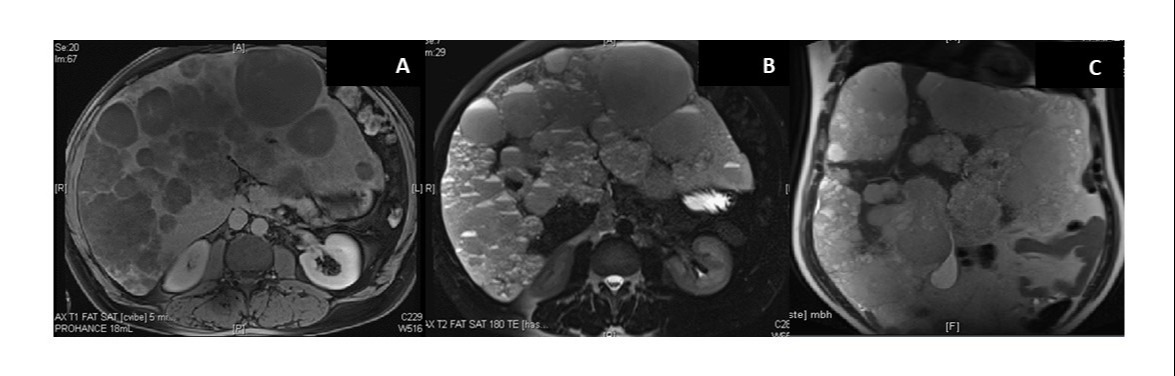
Figure: Figure 1: MR Abdomen with and without contrast showing hepatomegaly to 31cm (from 27cm two years prior) with innumerable hepatic lesions. Lesions demonstrated T2 hyperintense (figure 1B, 1C) and T1 hypointense signals (figure 1A) with partial diffusion restriction and central enhancement in many with slow delayed enhancement. Many demonstrated intrinsic hemorrhaging. A dominant lesion in the left hepatic lobe measured 9.5 x 8.7cm and was previously approximately 8.7 x 7cm. Also present is a severely narrowed left portal vein and left and middle hepatic veins. There was mild narrowing of the inferior vena cava.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zachary Vinton indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
Clark Kulig indicated no relevant financial relationships.
Zachary C. Vinton, DO1, Stephanie J. Melquist, MD, MPH2, Clark C. Kulig, MD3. P1267 - Isolated Polycystic Liver Disease Requiring Transplant- A Rare Indication for MELD Exception, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

