Sunday Poster Session
Category: Liver
P1276 - Resolution of Portal Hypertension in Cystic Fibrosis Liver Disease After Start of CFTR Modulator: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Erica Loon, DO
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Erica Loon, DO, Joanne Billings, MD, MPH, Nicholas Lim, MD
University of Minnesota Medical Center, Minneapolis, MN
Introduction: Portal hypertension (PH) secondary to cystic fibrosis liver disease (CFLD) is the third most common cause for mortality (after lung failure and lung transplantation) in adults with cystic fibrosis (CF). Notably, PH in CFLD more often occurs in absence of cirrhosis (i.e. non-cirrhotic PH, NCPH). Here, we describe a patient with NCPH secondary to CFLD with resolution of PH after starting a cystic fibrosis transmembrane conductance regulator (CFTR) modulator.
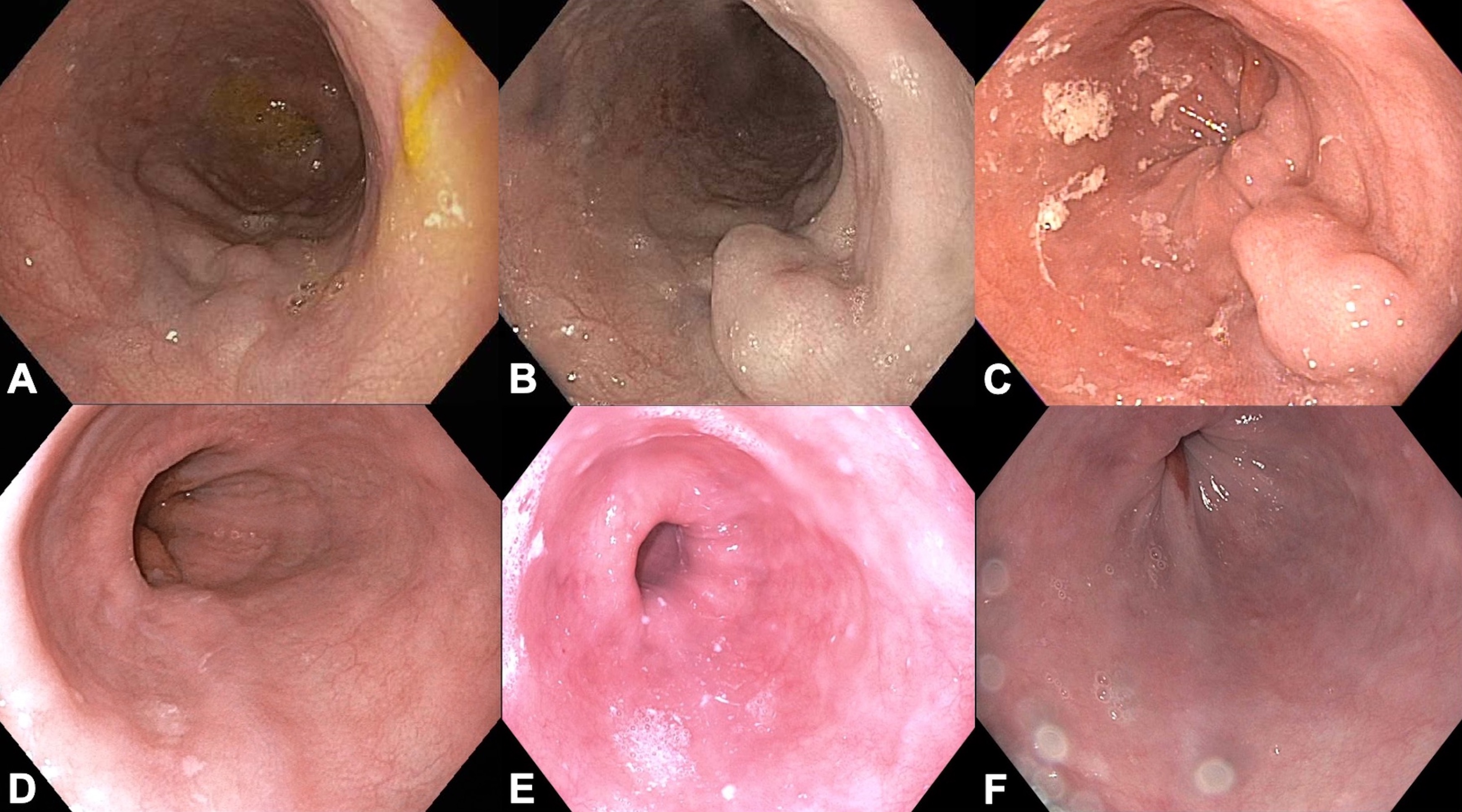
Case Description/Methods: A 73-year-old male diagnosed in 1964 with CF, homozygous F508del, characterized by ‘severe’ pulmonary obstruction and CF-related diabetes mellitus underwent lung transplant evaluation in 2015. Abdominal ultrasound revealed a nodular liver and splenomegaly (14.1 cm). Transjugular liver biopsy was non-diagnostic due to insufficient sampling, however, portosystemic gradient was elevated to 28 mmHg. Upper endoscopy (EGD) showed a single, grade I esophageal varix (Figure 1A). Follow-up EGDs showed esophageal varices, including a grade III varix requiring band ligation in 2018, and PH gastropathy (Figure 1B-D). Repeat biopsy confirmed portal and hepatic venous abnormalities and 3 mmHg portosystemic gradient, but no cirrhosis. The patient was declined listing for lung-liver transplant due to his advanced age and presence of PH.
In 2019, he was started on CFTR modulator tezacaftor/ivacaftor and ivacaftor. Six months later, the patient was switched to the newer elexacaftor/tezacaftor/ivacaftor (ETI). Eight weeks after starting ETI, he was off oxygen at rest. By month 10, he was off all oxygen and short-acting insulin, and swimming 1,000 feet daily. In 2021, 18 months after starting ETI, EGD revealed a normal esophagus and stomach with resolution of esophageal varices and PH gastropathy (Figure 1E). Ultrasound in 2022 again demonstrated a nodular liver but now with a normal-sized spleen (12.8 cm). EGD in 2023 confirmed absence of varices and gastropathy (Figure 1F). In December 2023, the patient was downgraded from ‘severe’ to ‘moderate’ pulmonary obstruction and achieving 20,000 steps per day.
Discussion: Information on the efficacy of CFTR modulators in patients with CFLD is limited. As demonstrated in this patient, CFTR modulators may provide extra-pulmonary benefits including reversal of NCPH. Long-term use of CFTR modulators could potentially result in reductions in mortality from PH and need for future liver or combined lung-liver transplantation in patients with CFLD.
Disclosures:
Erica Loon, DO, Joanne Billings, MD, MPH, Nicholas Lim, MD. P1276 - Resolution of Portal Hypertension in Cystic Fibrosis Liver Disease After Start of CFTR Modulator: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Minnesota Medical Center, Minneapolis, MN
Introduction: Portal hypertension (PH) secondary to cystic fibrosis liver disease (CFLD) is the third most common cause for mortality (after lung failure and lung transplantation) in adults with cystic fibrosis (CF). Notably, PH in CFLD more often occurs in absence of cirrhosis (i.e. non-cirrhotic PH, NCPH). Here, we describe a patient with NCPH secondary to CFLD with resolution of PH after starting a cystic fibrosis transmembrane conductance regulator (CFTR) modulator.
Case Description/Methods: A 73-year-old male diagnosed in 1964 with CF, homozygous F508del, characterized by ‘severe’ pulmonary obstruction and CF-related diabetes mellitus underwent lung transplant evaluation in 2015. Abdominal ultrasound revealed a nodular liver and splenomegaly (14.1 cm). Transjugular liver biopsy was non-diagnostic due to insufficient sampling, however, portosystemic gradient was elevated to 28 mmHg. Upper endoscopy (EGD) showed a single, grade I esophageal varix (Figure 1A). Follow-up EGDs showed esophageal varices, including a grade III varix requiring band ligation in 2018, and PH gastropathy (Figure 1B-D). Repeat biopsy confirmed portal and hepatic venous abnormalities and 3 mmHg portosystemic gradient, but no cirrhosis. The patient was declined listing for lung-liver transplant due to his advanced age and presence of PH.
In 2019, he was started on CFTR modulator tezacaftor/ivacaftor and ivacaftor. Six months later, the patient was switched to the newer elexacaftor/tezacaftor/ivacaftor (ETI). Eight weeks after starting ETI, he was off oxygen at rest. By month 10, he was off all oxygen and short-acting insulin, and swimming 1,000 feet daily. In 2021, 18 months after starting ETI, EGD revealed a normal esophagus and stomach with resolution of esophageal varices and PH gastropathy (Figure 1E). Ultrasound in 2022 again demonstrated a nodular liver but now with a normal-sized spleen (12.8 cm). EGD in 2023 confirmed absence of varices and gastropathy (Figure 1F). In December 2023, the patient was downgraded from ‘severe’ to ‘moderate’ pulmonary obstruction and achieving 20,000 steps per day.
Discussion: Information on the efficacy of CFTR modulators in patients with CFLD is limited. As demonstrated in this patient, CFTR modulators may provide extra-pulmonary benefits including reversal of NCPH. Long-term use of CFTR modulators could potentially result in reductions in mortality from PH and need for future liver or combined lung-liver transplantation in patients with CFLD.
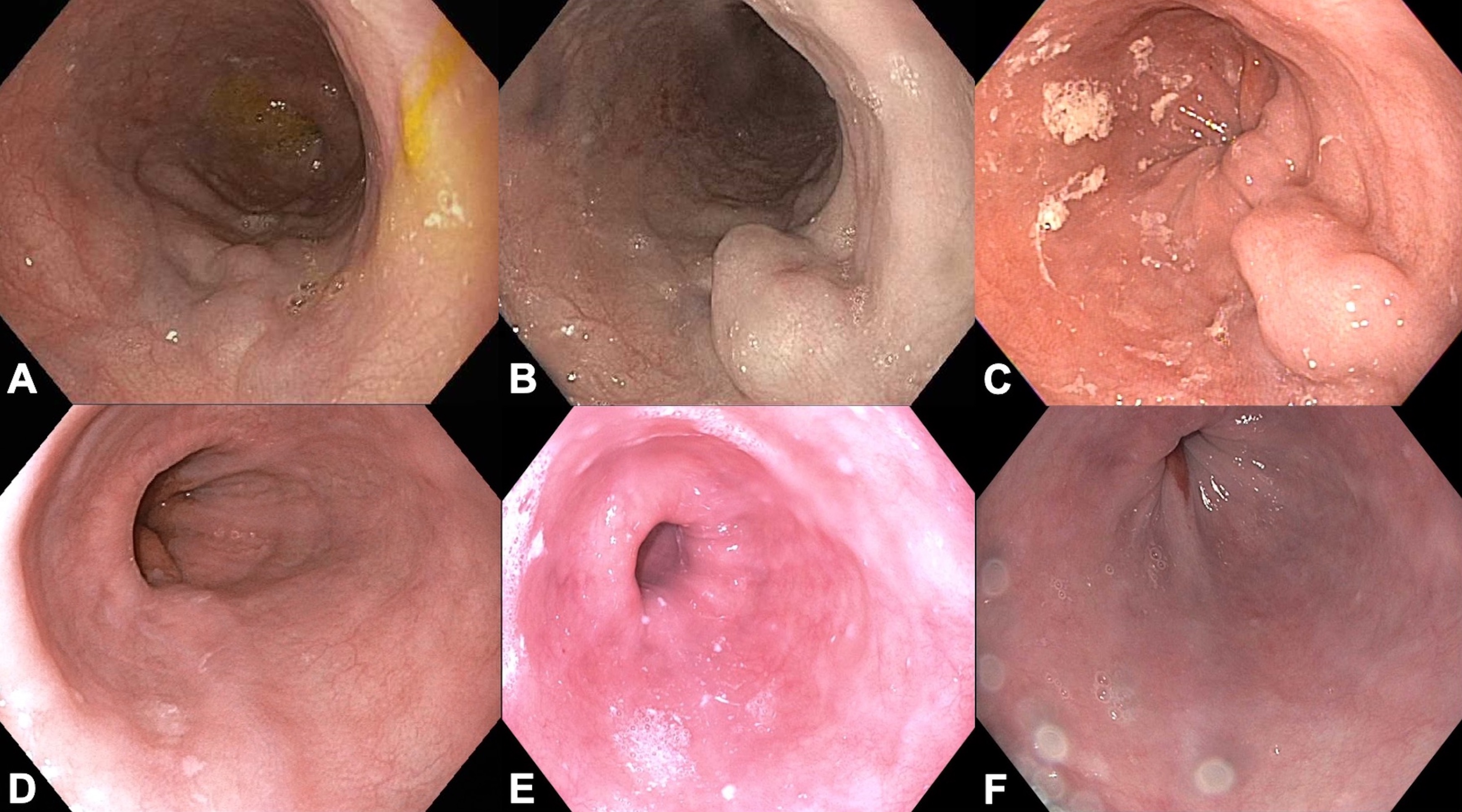
Figure: Figure 1A. Single, grade I esophageal varix (2015).
Figure 1B. Single, grade II esophageal varix (2017).
Figure 1C. Single column of grade III esophageal varix requiring band ligation (2018).
Figure 1D. Grade I esophageal varices (2019).
Figure 1E. Normal esophagus without varices (2021, 1.5 years after starting CFTR modulator).
Figure 1F. Normal esophagus without varices (2023, 3.5 years after starting CFTR modulator).
Figure 1B. Single, grade II esophageal varix (2017).
Figure 1C. Single column of grade III esophageal varix requiring band ligation (2018).
Figure 1D. Grade I esophageal varices (2019).
Figure 1E. Normal esophagus without varices (2021, 1.5 years after starting CFTR modulator).
Figure 1F. Normal esophagus without varices (2023, 3.5 years after starting CFTR modulator).
Disclosures:
Erica Loon indicated no relevant financial relationships.
Joanne Billings indicated no relevant financial relationships.
Nicholas Lim indicated no relevant financial relationships.
Erica Loon, DO, Joanne Billings, MD, MPH, Nicholas Lim, MD. P1276 - Resolution of Portal Hypertension in Cystic Fibrosis Liver Disease After Start of CFTR Modulator: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

