Sunday Poster Session
Category: Liver
P1306 - Unravelling the Puzzle: The Role of Transjugular Liver Biopsy in Hemophagocytic Syndrome with Liver involvement
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FM
Francisco Mendes, MD
Centro Hospitalar Universitário de São João
Porto, Porto, Portugal
Presenting Author(s)
Francisco Mendes, MD1, Tiago Ribeiro, MD1, Susana Lopes, MD, PhD, FACG1, Elsa Fonseca, MD, PhD2, Guilherme Macedo, MD, PhD, FACG1
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2Centro Hospitalar Universitário São João, Porto, Porto, Portugal
Introduction: Transjugular liver biopsy is a useful procedure in patients with contraindication for conventional percutaneous liver biopsy. Indeed, this diagnostic procedure is of utmost importance in specific cases, namely in patients with hematological disorders who require liver biopsy.
Case Description/Methods: A 64-year-old female with no relevant medical history presented to the emergency department with a 3-week history of fever, malaise and headache, associated with jaundice with 3 days of evolution. The epidemiologic history was irrelevant. Due to hypotension unresponsive to fluids, the patient was admitted to the intensive care unit on vasopressors and large spectrum antibiotics.
The lab values revealed pancytopenia (hemoglobin 9.6g/dL, leucocytes 0.85x109/L and platelets 43x109/L), coagulopathy (with a prothrombin time of 20 seconds) and cholestatic hepatitis (R-Factor 1.7, with alanine transaminase 10 times and alkaline phosphatase 6 times the reference values). The patient had a direct hiperbilirrubinemia with a total bilirubin of 6.6mg/dL. Additionally, an hyperinflammatory state was objectified, with lactate desidrogenase of 4900U/L, serum ferritin of 15000U/L and C-reactive protein of 15mg/L. A contrast-enhanced abdominal computerized tomography revealed multiple infracentrimetric liver nodules.
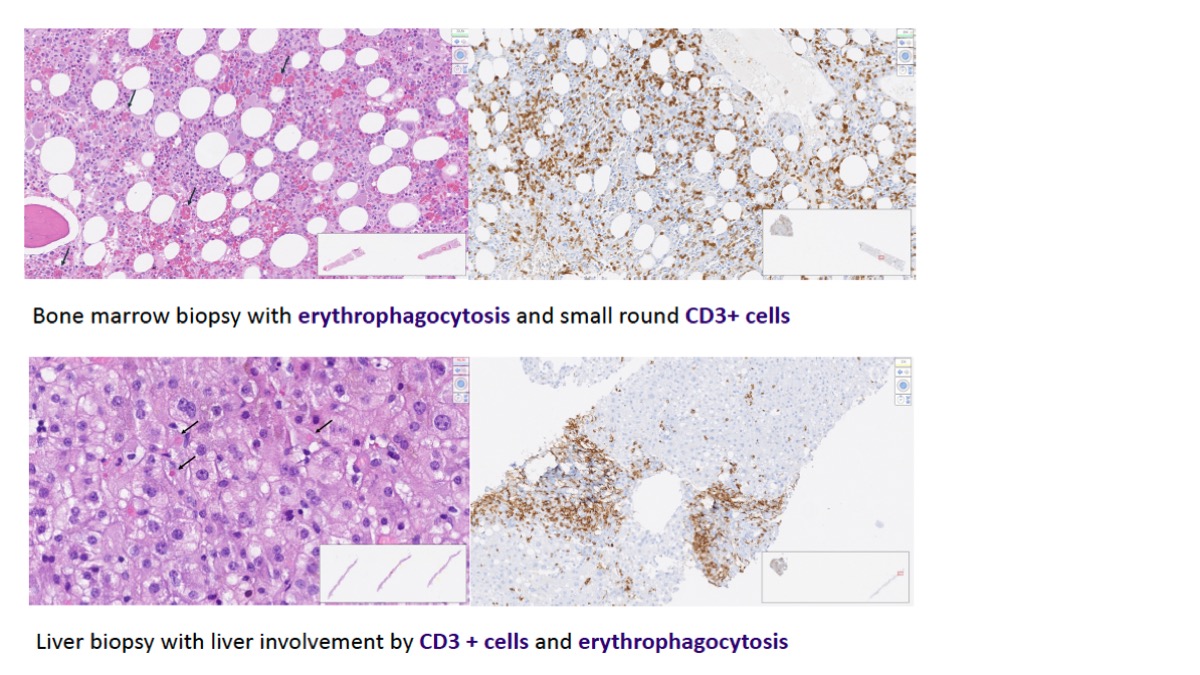
Due to high clinical suspicion of hemophagocytic syndrome, the patient underwent transjugular liver biopsy, bone marrow biopsy and initiated dexamethasone. Liver biopsy revealed infiltration by monoclonal T-cells, associated with erythrophagocytosis, confirmed by bone marrow biopsy. The patient initiated chemotherapy with cyclophosphamide, gemcitabine and vincristine (in concordance with the diagnosis of T-cell lymphoma). It was observed a progressive clinical improvement with normalization of bilirubin, regression of cytolysis and cholestasis, and the patient was referred to outpatient Hematology clinic after discharge.
Discussion: Hemophagocytic or macrophage activation syndrome results from immunological hyperactivation with macrophage-mediated multiorgan failure. It develops in a genetic context or secondary to infections, autoimmune diseases or malignancies. The presence of predominant liver involvement is rare and liver biopsy is essential in the diagnostic workup. This clinical case demonstrates liver damage mediated by both hemophagocytic syndrome and liver involvement by a T-cell lymphoma, showing the importance of high clinical suspicion for a prompt diagnosis.
Disclosures:
Francisco Mendes, MD1, Tiago Ribeiro, MD1, Susana Lopes, MD, PhD, FACG1, Elsa Fonseca, MD, PhD2, Guilherme Macedo, MD, PhD, FACG1. P1306 - Unravelling the Puzzle: The Role of Transjugular Liver Biopsy in Hemophagocytic Syndrome with Liver involvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2Centro Hospitalar Universitário São João, Porto, Porto, Portugal
Introduction: Transjugular liver biopsy is a useful procedure in patients with contraindication for conventional percutaneous liver biopsy. Indeed, this diagnostic procedure is of utmost importance in specific cases, namely in patients with hematological disorders who require liver biopsy.
Case Description/Methods: A 64-year-old female with no relevant medical history presented to the emergency department with a 3-week history of fever, malaise and headache, associated with jaundice with 3 days of evolution. The epidemiologic history was irrelevant. Due to hypotension unresponsive to fluids, the patient was admitted to the intensive care unit on vasopressors and large spectrum antibiotics.
The lab values revealed pancytopenia (hemoglobin 9.6g/dL, leucocytes 0.85x109/L and platelets 43x109/L), coagulopathy (with a prothrombin time of 20 seconds) and cholestatic hepatitis (R-Factor 1.7, with alanine transaminase 10 times and alkaline phosphatase 6 times the reference values). The patient had a direct hiperbilirrubinemia with a total bilirubin of 6.6mg/dL. Additionally, an hyperinflammatory state was objectified, with lactate desidrogenase of 4900U/L, serum ferritin of 15000U/L and C-reactive protein of 15mg/L. A contrast-enhanced abdominal computerized tomography revealed multiple infracentrimetric liver nodules.
Due to high clinical suspicion of hemophagocytic syndrome, the patient underwent transjugular liver biopsy, bone marrow biopsy and initiated dexamethasone. Liver biopsy revealed infiltration by monoclonal T-cells, associated with erythrophagocytosis, confirmed by bone marrow biopsy. The patient initiated chemotherapy with cyclophosphamide, gemcitabine and vincristine (in concordance with the diagnosis of T-cell lymphoma). It was observed a progressive clinical improvement with normalization of bilirubin, regression of cytolysis and cholestasis, and the patient was referred to outpatient Hematology clinic after discharge.
Discussion: Hemophagocytic or macrophage activation syndrome results from immunological hyperactivation with macrophage-mediated multiorgan failure. It develops in a genetic context or secondary to infections, autoimmune diseases or malignancies. The presence of predominant liver involvement is rare and liver biopsy is essential in the diagnostic workup. This clinical case demonstrates liver damage mediated by both hemophagocytic syndrome and liver involvement by a T-cell lymphoma, showing the importance of high clinical suspicion for a prompt diagnosis.
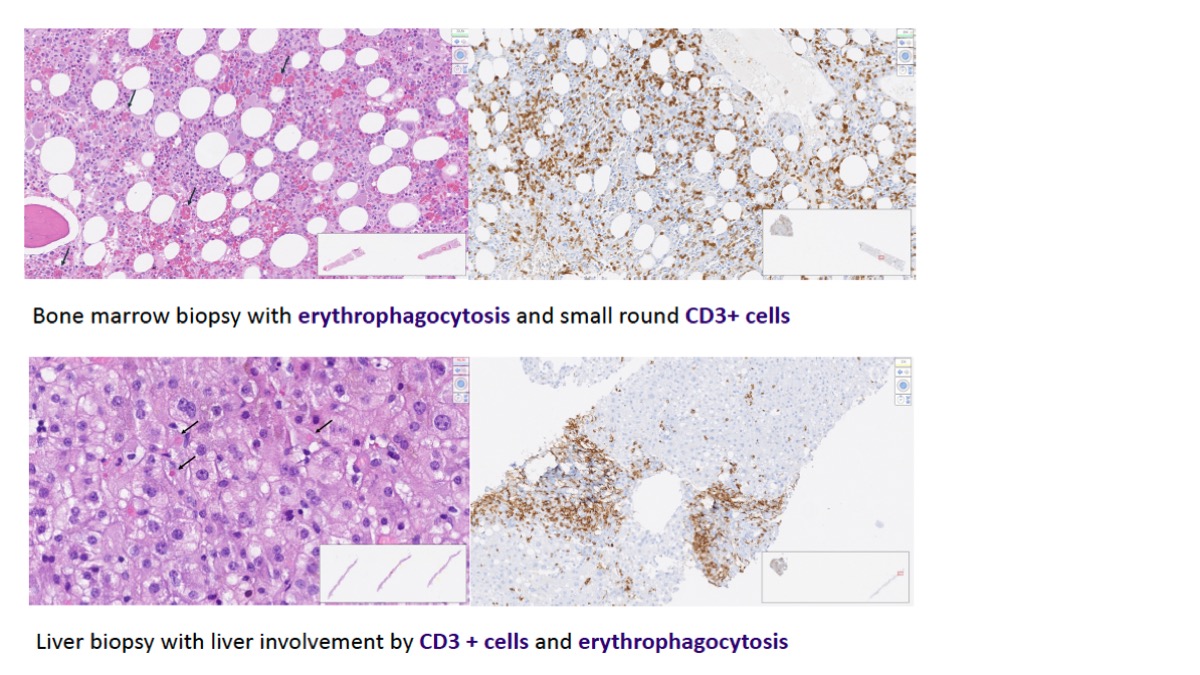
Figure: Figure 1 - Bone marrow and liver biopsy in patient with pancytopenia and cholestatic hepatitis.
Disclosures:
Francisco Mendes indicated no relevant financial relationships.
Tiago Ribeiro indicated no relevant financial relationships.
Susana Lopes indicated no relevant financial relationships.
Elsa Fonseca indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Francisco Mendes, MD1, Tiago Ribeiro, MD1, Susana Lopes, MD, PhD, FACG1, Elsa Fonseca, MD, PhD2, Guilherme Macedo, MD, PhD, FACG1. P1306 - Unravelling the Puzzle: The Role of Transjugular Liver Biopsy in Hemophagocytic Syndrome with Liver involvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
