Sunday Poster Session
Category: Liver
P1311 - Diabetic Hepatosclerosis: An Emerging Cause of Portal Hypertension
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Manuela Araque, MD, MPH
University of Miami/Jackson Medical Hospital
Miami, FL
Presenting Author(s)
Manuela Araque, MD, MPH1, Sally Condon, MD2, Elizabeth Montgomery, MD2, Francesco Alessandrino, MD2, Jessica Kumar, MD2, Joshua Turkeltaub, MD2, Patricia Jones, MD, MSCR2
1University of Miami/Jackson Medical Hospital, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Diabetic hepatosclerosis is a rare, recently recognized microangiopathic complication of diabetes mellitus. It is thought to mainly affect patients with long-standing insulin-dependent diabetes with coexisting microvascular complications, such as nephropathy. In most reported cases, patients are asymptomatic from a liver standpoint. The risk and rate of progression to cirrhosis from this rarely recognized entity is unknown.
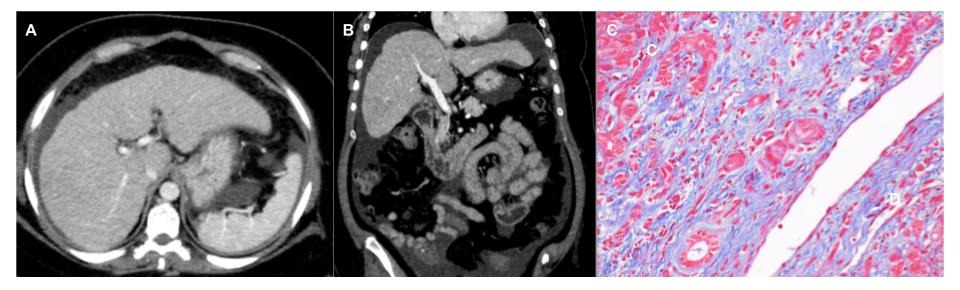
Case Description/Methods: A 38-year-old female with a two-year history of non-insulin dependent diabetes mellitus presented to the emergency room due to a month-long history of abdominal distension. Liver transaminases were mildly elevated, but alkaline phosphatase (476 IU/l) and gamma-glutamyl transferase (815 IU/L) were significantly elevated. CT of the abdomen suggested a new diagnosis of cirrhosis (Figure 1A and 1B). Paracentesis was performed and fluid analysis showing high SAAG ( >1.1) and low protein (< 2.5) ascites, consistent with portal hypertension. MELD score was 12 (Table 1).
A workup for chronic liver disease was indeterminate for a definitive cause. Anti-smooth muscle antibody (ASMA) was weakly positive, but IgG was normal. All other work up was negative. Given underlying diabetes and obesity, she was presumed to have cirrhosis from metabolic-associated steatotic liver disease (MASLD). Liver biopsy was performed to exclude autoimmune hepatitis and investigate her cholestasis. Transjugular liver biopsy revealed free hepatic venous pressure of 10 mm Hg and wedged hepatic venous pressure of 30 mm Hg. Biopsy revealed perisinusoidal fibrosis, diabetic vascular changes with sclerosis of arteries, duct injury, and extensive ductular reaction with mild steatosis (5%), consistent with diabetic hepatosclerosis and a separate area of band-like fibrosis with regenerative nodule formation suggesting evolving cirrhosis (Figure 1C). Following symptomatic improvement, the patient was discharged on diuretics to manage her ascites.
Discussion: In this patient presumed to have cirrhosis from MASLD, diabetic hepatosclerosis was noted on biopsy, highlighting the importance of histological evaluation in atypical cases. Diabetic hepatosclerosis is extremely rare and there is limited data regarding predisposing factors, proposed management, and long-term outcomes. Likely, diabetic hepatosclerosis is underdiagnosed. Future studies should seek to determine the epidemiological and genetic risk factors for diabetic hepatosclerosis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Manuela Araque, MD, MPH1, Sally Condon, MD2, Elizabeth Montgomery, MD2, Francesco Alessandrino, MD2, Jessica Kumar, MD2, Joshua Turkeltaub, MD2, Patricia Jones, MD, MSCR2. P1311 - Diabetic Hepatosclerosis: An Emerging Cause of Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami/Jackson Medical Hospital, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Diabetic hepatosclerosis is a rare, recently recognized microangiopathic complication of diabetes mellitus. It is thought to mainly affect patients with long-standing insulin-dependent diabetes with coexisting microvascular complications, such as nephropathy. In most reported cases, patients are asymptomatic from a liver standpoint. The risk and rate of progression to cirrhosis from this rarely recognized entity is unknown.
Case Description/Methods: A 38-year-old female with a two-year history of non-insulin dependent diabetes mellitus presented to the emergency room due to a month-long history of abdominal distension. Liver transaminases were mildly elevated, but alkaline phosphatase (476 IU/l) and gamma-glutamyl transferase (815 IU/L) were significantly elevated. CT of the abdomen suggested a new diagnosis of cirrhosis (Figure 1A and 1B). Paracentesis was performed and fluid analysis showing high SAAG ( >1.1) and low protein (< 2.5) ascites, consistent with portal hypertension. MELD score was 12 (Table 1).
A workup for chronic liver disease was indeterminate for a definitive cause. Anti-smooth muscle antibody (ASMA) was weakly positive, but IgG was normal. All other work up was negative. Given underlying diabetes and obesity, she was presumed to have cirrhosis from metabolic-associated steatotic liver disease (MASLD). Liver biopsy was performed to exclude autoimmune hepatitis and investigate her cholestasis. Transjugular liver biopsy revealed free hepatic venous pressure of 10 mm Hg and wedged hepatic venous pressure of 30 mm Hg. Biopsy revealed perisinusoidal fibrosis, diabetic vascular changes with sclerosis of arteries, duct injury, and extensive ductular reaction with mild steatosis (5%), consistent with diabetic hepatosclerosis and a separate area of band-like fibrosis with regenerative nodule formation suggesting evolving cirrhosis (Figure 1C). Following symptomatic improvement, the patient was discharged on diuretics to manage her ascites.
Discussion: In this patient presumed to have cirrhosis from MASLD, diabetic hepatosclerosis was noted on biopsy, highlighting the importance of histological evaluation in atypical cases. Diabetic hepatosclerosis is extremely rare and there is limited data regarding predisposing factors, proposed management, and long-term outcomes. Likely, diabetic hepatosclerosis is underdiagnosed. Future studies should seek to determine the epidemiological and genetic risk factors for diabetic hepatosclerosis.
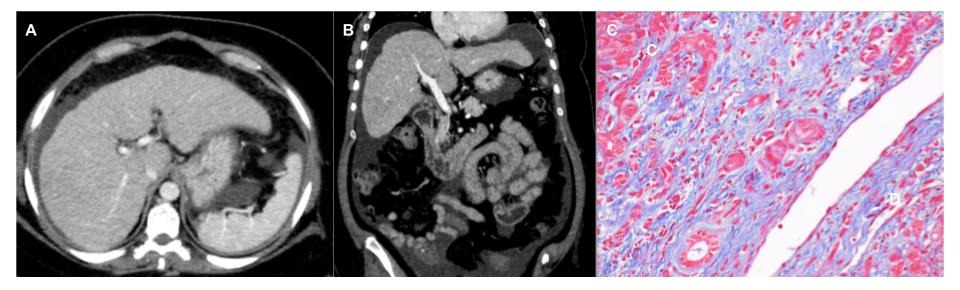
Figure: Figure 1: Axial (A) and coronal (B) CT images of the liver obtained during portal venous phase demonstrate nodular contour of the liver (arrow) and prominence of the lateral segments of the left liver lobe (arrowhead), findings observed in cirrhosis, as well as moderate volume ascites (curved arrows). Perisinusoidal fibrosis, diabetic vascular changes with sclerosis of arteries, duct injury, and extensive ductular reaction with mild steatosis (5%) and a separate area of band-like fibrosis with regenerative nodule formation suggesting evolving cirrhosis portrayed in Figure 1C.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Manuela Araque indicated no relevant financial relationships.
Sally Condon indicated no relevant financial relationships.
Elizabeth Montgomery indicated no relevant financial relationships.
Francesco Alessandrino: Ascelia Pharma – Subinvestigator.
Jessica Kumar indicated no relevant financial relationships.
Joshua Turkeltaub indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Manuela Araque, MD, MPH1, Sally Condon, MD2, Elizabeth Montgomery, MD2, Francesco Alessandrino, MD2, Jessica Kumar, MD2, Joshua Turkeltaub, MD2, Patricia Jones, MD, MSCR2. P1311 - Diabetic Hepatosclerosis: An Emerging Cause of Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
