Sunday Poster Session
Category: Liver
P1319 - Defibrotide and Plasmapheresis to Treat Hepatic Sinusoidal Obstruction Syndrome in a Patient with Acute Lymphoblastic Leukemia on PEG-Asparaginase
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Joshua P. Thariath, MD, MS
McGaw Medical Center of Northwestern University
Chicago, IL
Presenting Author(s)
Joshua Thariath, MD, MS, Daniel McLoughlin, BA
McGaw Medical Center of Northwestern University, Chicago, IL
Introduction: Sinusoidal obstruction syndrome (SOS) is caused by damage to hepatic sinusoidal endothelial cells, leading to liver injury and potential liver and multi-organ failure. Though chemotherapeutic agents are among the known causes, SOS is most seen following hematopoietic stem cell transplant. The only approved therapy, defibrotide, works by encouraging fibrinolysis and reducing endothelial cell activation. Plasmapheresis has been used previously to treat conditions characterized by microvascular thromboses by removing fibrinogen, as well as in patients with acute liver failure to remove ammonia and other toxic waste products that are not cleared. Both therapies were employed to treat the following patient, which led to survival in an initially poor prognosis case.
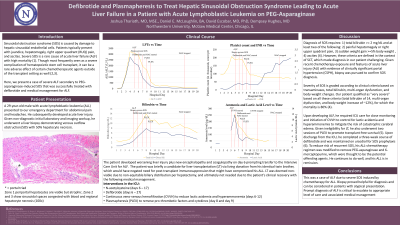
Case Description/Methods: A 29-year-old male with acute lymphoblastic leukemia on CALGB-10403 induction chemotherapy, which includes PEG-asparaginase, presented for abdominal pain and headaches. Though workup was initially unrevealing, he subsequently developed acute liver injury. He underwent liver biopsy which was consistent with venous outflow obstruction/SOS with 50% hepatocyte necrosis. He then developed asterixis, jaundice, and confusion concerning for hepatic encephalopathy and was transferred to the ICU for acute liver failure. Liver function tests peaked at AST/ALT 2511/3339, and total bilirubin/direct bilirubin peaked at 15.9/8.6. He was started on defibrotide for SOS as well as continuous veno-venous hemofiltration for hepatorenal/shock-related kidney injury. Plasmapheresis was initiated for hyperammonemia and to remove pro-thrombotic factors and cytokines. He was evaluated for liver transplant, but he improved with treatment and was transferred to the floor. His liver and kidney function continued to improve, and he underwent multiple paracenteses for comfort. He completed 21 days of defibrotide and was discharged on spironolactone and furosemide to prevent reaccumulation of ascites.
Discussion: This case involves a rare presentation of SOS outside the context of stem cell transplant and shows the relationship between commonly implicated chemotherapeutic regimens and SOS, the high morbidity once patients develop multi-organ failure, and the established role of defibrotide. It also illustrates the role of plasmapheresis in this condition as well as acute liver failure. Fortunately, this was a rare case where the patient survived with normalized markers of organ function and a good prognosis.
Disclosures:
Joshua Thariath, MD, MS, Daniel McLoughlin, BA. P1319 - Defibrotide and Plasmapheresis to Treat Hepatic Sinusoidal Obstruction Syndrome in a Patient with Acute Lymphoblastic Leukemia on PEG-Asparaginase, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
McGaw Medical Center of Northwestern University, Chicago, IL
Introduction: Sinusoidal obstruction syndrome (SOS) is caused by damage to hepatic sinusoidal endothelial cells, leading to liver injury and potential liver and multi-organ failure. Though chemotherapeutic agents are among the known causes, SOS is most seen following hematopoietic stem cell transplant. The only approved therapy, defibrotide, works by encouraging fibrinolysis and reducing endothelial cell activation. Plasmapheresis has been used previously to treat conditions characterized by microvascular thromboses by removing fibrinogen, as well as in patients with acute liver failure to remove ammonia and other toxic waste products that are not cleared. Both therapies were employed to treat the following patient, which led to survival in an initially poor prognosis case.
Case Description/Methods: A 29-year-old male with acute lymphoblastic leukemia on CALGB-10403 induction chemotherapy, which includes PEG-asparaginase, presented for abdominal pain and headaches. Though workup was initially unrevealing, he subsequently developed acute liver injury. He underwent liver biopsy which was consistent with venous outflow obstruction/SOS with 50% hepatocyte necrosis. He then developed asterixis, jaundice, and confusion concerning for hepatic encephalopathy and was transferred to the ICU for acute liver failure. Liver function tests peaked at AST/ALT 2511/3339, and total bilirubin/direct bilirubin peaked at 15.9/8.6. He was started on defibrotide for SOS as well as continuous veno-venous hemofiltration for hepatorenal/shock-related kidney injury. Plasmapheresis was initiated for hyperammonemia and to remove pro-thrombotic factors and cytokines. He was evaluated for liver transplant, but he improved with treatment and was transferred to the floor. His liver and kidney function continued to improve, and he underwent multiple paracenteses for comfort. He completed 21 days of defibrotide and was discharged on spironolactone and furosemide to prevent reaccumulation of ascites.
Discussion: This case involves a rare presentation of SOS outside the context of stem cell transplant and shows the relationship between commonly implicated chemotherapeutic regimens and SOS, the high morbidity once patients develop multi-organ failure, and the established role of defibrotide. It also illustrates the role of plasmapheresis in this condition as well as acute liver failure. Fortunately, this was a rare case where the patient survived with normalized markers of organ function and a good prognosis.
Disclosures:
Joshua Thariath indicated no relevant financial relationships.
Daniel McLoughlin indicated no relevant financial relationships.
Joshua Thariath, MD, MS, Daniel McLoughlin, BA. P1319 - Defibrotide and Plasmapheresis to Treat Hepatic Sinusoidal Obstruction Syndrome in a Patient with Acute Lymphoblastic Leukemia on PEG-Asparaginase, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
