Sunday Poster Session
Category: Liver
P1332 - To Be or Not to Be? Segmental Atrophy of the Liver Disguised as Malignancy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Marilee Tiru-Vega, MD
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Marilee Tirú-Vega, MD, Ricardo Lopez-Valle, MD, Kathia Rosado-Orozco, MD, Andres Rabell-Bernal, MD
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Segmental atrophy of the liver is a rare clinical entity most attributed to focal vascular injury of the hepatic parenchyma resulting in a hepatic pseudotumor. Due to its strong resemblance to hepatic malignancies on imaging, diagnosis poses a clinical challenge only achieved via direct tissue sampling. In the case below, we present a patient with imaging findings concerning for malignancy, later identified as a hepatic pseudotumor.
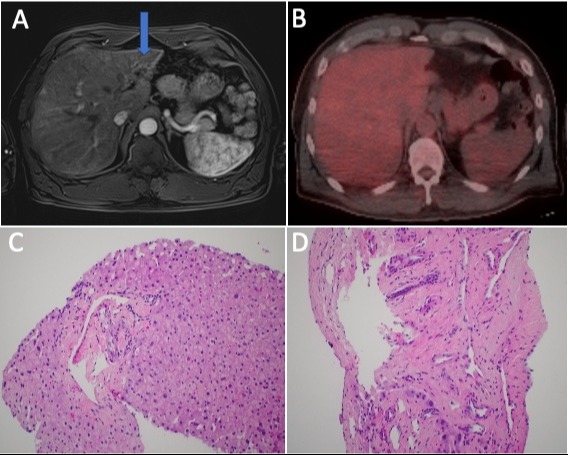
Case Description/Methods: A 52-year-old male patient with history of follicular thyroid cancer status-post thyroidectomy presents with progressive, nonspecific, right upper quadrant abdominal discomfort. Denied associated symptoms such as fever, diarrhea, undesired weight loss, dyspepsia, biliary colic, yellowing of skin, acholic stools, mucocutaneous ulcers or dark urine. Abdominopelvic CT demonstrated a hypodense lesion in the hepatic segment II further characterized by MRI suspicious for a cholangiocarcinoma. Liver chemistries and tumor markers were within normal limits. PET/CT did not show an FDG avid lesion suggesting either a benign or a low mitotic rate lesion. Thus, the differential diagnosis was broad and hepatic tissue biopsy became paramount for establishing definitive diagnosis. Histopathology demonstrated subcapsular elasto-fibromatous changes; no dysplasia or steatosis were seen. In light of this, the patient’s clinical, radiologic and histopathologic presentation was most consistent with segmental atrophy of the liver causing a hepatic pseudotumor.
Discussion: Hepatic pseudotumor secondary to segmental atrophy and nodular elastosis remains a rare, yet benign, entity with a wide spectrum of differential diagnosis; malignancy being the most feared. Initially characterized as hepatic masses on imaging studies, on FDG-PET/CT, the lesions demonstrate iso-metabolism in comparison to the background hepatic parenchyma, suggesting their benign nature. Ischemic injury is thought to be the culprit leading to the production of elastic fibers and eventual nodular elastosis identified histologically. Management is conservative and only requires localized resection if symptomatic. Serial radiologic studies are not recommended unless there are concerning clinical symptoms for malignancy or abnormalities in liver chemistries. This case highlights the importance of considering hepatic pseudotumors in the differential diagnosis of hepatic masses as prompt tissue diagnosis is crucial for avoiding more invasive interventions thus improving patient morbidity.
Disclosures:
Marilee Tirú-Vega, MD, Ricardo Lopez-Valle, MD, Kathia Rosado-Orozco, MD, Andres Rabell-Bernal, MD. P1332 - To Be or Not to Be? Segmental Atrophy of the Liver Disguised as Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Segmental atrophy of the liver is a rare clinical entity most attributed to focal vascular injury of the hepatic parenchyma resulting in a hepatic pseudotumor. Due to its strong resemblance to hepatic malignancies on imaging, diagnosis poses a clinical challenge only achieved via direct tissue sampling. In the case below, we present a patient with imaging findings concerning for malignancy, later identified as a hepatic pseudotumor.
Case Description/Methods: A 52-year-old male patient with history of follicular thyroid cancer status-post thyroidectomy presents with progressive, nonspecific, right upper quadrant abdominal discomfort. Denied associated symptoms such as fever, diarrhea, undesired weight loss, dyspepsia, biliary colic, yellowing of skin, acholic stools, mucocutaneous ulcers or dark urine. Abdominopelvic CT demonstrated a hypodense lesion in the hepatic segment II further characterized by MRI suspicious for a cholangiocarcinoma. Liver chemistries and tumor markers were within normal limits. PET/CT did not show an FDG avid lesion suggesting either a benign or a low mitotic rate lesion. Thus, the differential diagnosis was broad and hepatic tissue biopsy became paramount for establishing definitive diagnosis. Histopathology demonstrated subcapsular elasto-fibromatous changes; no dysplasia or steatosis were seen. In light of this, the patient’s clinical, radiologic and histopathologic presentation was most consistent with segmental atrophy of the liver causing a hepatic pseudotumor.
Discussion: Hepatic pseudotumor secondary to segmental atrophy and nodular elastosis remains a rare, yet benign, entity with a wide spectrum of differential diagnosis; malignancy being the most feared. Initially characterized as hepatic masses on imaging studies, on FDG-PET/CT, the lesions demonstrate iso-metabolism in comparison to the background hepatic parenchyma, suggesting their benign nature. Ischemic injury is thought to be the culprit leading to the production of elastic fibers and eventual nodular elastosis identified histologically. Management is conservative and only requires localized resection if symptomatic. Serial radiologic studies are not recommended unless there are concerning clinical symptoms for malignancy or abnormalities in liver chemistries. This case highlights the importance of considering hepatic pseudotumors in the differential diagnosis of hepatic masses as prompt tissue diagnosis is crucial for avoiding more invasive interventions thus improving patient morbidity.
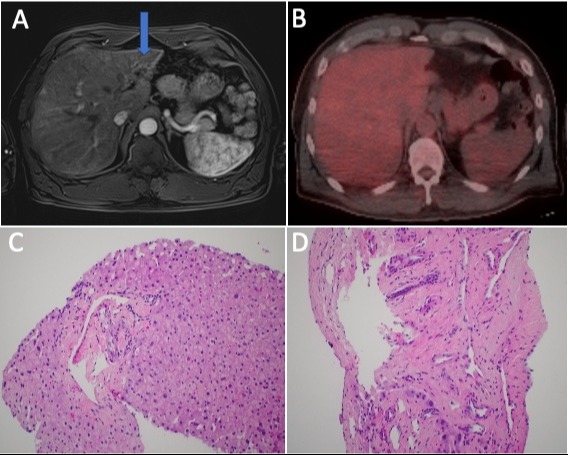
Figure: Figure 1A: Abdominopelvic MRI showing a T2 hypodense lesion (blue arrow) with progressive arterial enhancement at hepatic segment II, grossly measuring 2.1 cm anterior-posteriorly x 1.8 cm transversely.
1B: PET-CT showing no significant FDG avid lesion. Liver lesion on the left hepatic lobe does not show increased metabolic activity above the normal physiologic hepatic uptake.
1C: Histology of the left hepatic lesion core needle biopsy with hematoxylin and eosin (H&E) staining showing no dysplasia, microorganisms or steatosis.
1D: Histology of left hepatic lesion core needle biopsy with hematoxylin and eosin (H&E) staining showing extinction of hepatocytes with subscapular elasto-fibromatous changes.
1B: PET-CT showing no significant FDG avid lesion. Liver lesion on the left hepatic lobe does not show increased metabolic activity above the normal physiologic hepatic uptake.
1C: Histology of the left hepatic lesion core needle biopsy with hematoxylin and eosin (H&E) staining showing no dysplasia, microorganisms or steatosis.
1D: Histology of left hepatic lesion core needle biopsy with hematoxylin and eosin (H&E) staining showing extinction of hepatocytes with subscapular elasto-fibromatous changes.
Disclosures:
Marilee Tirú-Vega indicated no relevant financial relationships.
Ricardo Lopez-Valle indicated no relevant financial relationships.
Kathia Rosado-Orozco indicated no relevant financial relationships.
Andres Rabell-Bernal indicated no relevant financial relationships.
Marilee Tirú-Vega, MD, Ricardo Lopez-Valle, MD, Kathia Rosado-Orozco, MD, Andres Rabell-Bernal, MD. P1332 - To Be or Not to Be? Segmental Atrophy of the Liver Disguised as Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
