Sunday Poster Session
Category: Liver
P1334 - Double the Trouble: DILI and HAV Cause Significant Cholestatic Liver Injury
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hannah Laird, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Hannah Laird, MD, Laura E. Lavette, MD, Himesh Zaver, MD, Neeral Shah, MD
University of Virginia Medical Center, Charlottesville, VA
Introduction: Acute cholestatic liver injury has many causes but is usually associated with biliary obstruction or drug-induced liver injury (DILI). A thorough history is imperative to diagnosing the cause and guiding treatment. We present a unique case of cholestatic liver injury due to doxycycline-induced DILI and acute hepatitis A (HAV) infection.
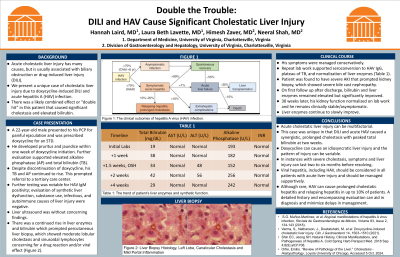
Case Description/Methods: A 22-year-old male presented to his primary care provider (PCP) for painful ejaculation and was prescribed a 7-day course of doxycycline for a sexually transmitted infection. He developed pruritus and jaundice within a week of doxycycline initiation. Further evaluation showed elevated alkaline phosphatase (AP) and total bilirubin (TB). Despite discontinuation of doxycycline, his TB and AP continued to rise, prompting referral to a tertiary care center for further evaluation. Elements of his social, medical, and travel history were unremarkable other than doxycycline initiation. Initial work-up was notable for HAV IgM positivity; evaluation of synthetic liver dysfunction, substance use, infectious, and autoimmune causes of liver injury were negative. Liver ultrasound was without concerning findings. There was a continued rise in liver enzymes and bilirubin which prompted percutaneous liver biopsy. Biopsy showed moderate lobular cholestasis and sinusoidal lymphocytes concerning for a drug reaction and/or viral effect. His symptoms were managed supportively. Repeat lab work confirmed seroconversion to HAV IgG, plateau of TB, stabilization of AP, and normalization of AST and ALT within one month (Table 1).
Discussion: Doxycycline can cause an idiosyncratic liver injury. In instances with severe cholestasis, symptoms and liver injury can last two to six months before resolving. Viral hepatitis, including HAV, should be considered in all patients with acute liver injury. Although rare, HAV can cause prolonged cholestatic hepatitis and relapsing hepatitis in up to 10% of patients during the first few months after acute illness. Our case underscores the importance of a detailed history and thorough work-up in appropriately diagnosing and treating multifactorial liver injuries.
S.G. Muñoz-Martínez, et al. Atypical manifestations of hepatitis A virus infection, Revista de Gastroenterología de México, Volume 83, Issue 2, 134-143 (2018).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hannah Laird, MD, Laura E. Lavette, MD, Himesh Zaver, MD, Neeral Shah, MD. P1334 - Double the Trouble: DILI and HAV Cause Significant Cholestatic Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Virginia Medical Center, Charlottesville, VA
Introduction: Acute cholestatic liver injury has many causes but is usually associated with biliary obstruction or drug-induced liver injury (DILI). A thorough history is imperative to diagnosing the cause and guiding treatment. We present a unique case of cholestatic liver injury due to doxycycline-induced DILI and acute hepatitis A (HAV) infection.
Case Description/Methods: A 22-year-old male presented to his primary care provider (PCP) for painful ejaculation and was prescribed a 7-day course of doxycycline for a sexually transmitted infection. He developed pruritus and jaundice within a week of doxycycline initiation. Further evaluation showed elevated alkaline phosphatase (AP) and total bilirubin (TB). Despite discontinuation of doxycycline, his TB and AP continued to rise, prompting referral to a tertiary care center for further evaluation. Elements of his social, medical, and travel history were unremarkable other than doxycycline initiation. Initial work-up was notable for HAV IgM positivity; evaluation of synthetic liver dysfunction, substance use, infectious, and autoimmune causes of liver injury were negative. Liver ultrasound was without concerning findings. There was a continued rise in liver enzymes and bilirubin which prompted percutaneous liver biopsy. Biopsy showed moderate lobular cholestasis and sinusoidal lymphocytes concerning for a drug reaction and/or viral effect. His symptoms were managed supportively. Repeat lab work confirmed seroconversion to HAV IgG, plateau of TB, stabilization of AP, and normalization of AST and ALT within one month (Table 1).
Discussion: Doxycycline can cause an idiosyncratic liver injury. In instances with severe cholestasis, symptoms and liver injury can last two to six months before resolving. Viral hepatitis, including HAV, should be considered in all patients with acute liver injury. Although rare, HAV can cause prolonged cholestatic hepatitis and relapsing hepatitis in up to 10% of patients during the first few months after acute illness. Our case underscores the importance of a detailed history and thorough work-up in appropriately diagnosing and treating multifactorial liver injuries.
S.G. Muñoz-Martínez, et al. Atypical manifestations of hepatitis A virus infection, Revista de Gastroenterología de México, Volume 83, Issue 2, 134-143 (2018).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hannah Laird indicated no relevant financial relationships.
Laura Lavette indicated no relevant financial relationships.
Himesh Zaver indicated no relevant financial relationships.
Neeral Shah indicated no relevant financial relationships.
Hannah Laird, MD, Laura E. Lavette, MD, Himesh Zaver, MD, Neeral Shah, MD. P1334 - Double the Trouble: DILI and HAV Cause Significant Cholestatic Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
