Sunday Poster Session
Category: Liver
P1337 - A Rare Case of Fluid Overload-Associated Large B Cell Lymphoma in a Patient With Hepatitis C Cirrhosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sanjna Shelukar, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Sanjna Shelukar, MD1, Amit Agarwal, MD2, Jonathan Gross, MD2, David Truscello, DO3, Elizaveta Flerova, MD2, Quinto Gesiotto, MD2, Onder Alpdogan, MD2, Jesse M. Civan, MD2, David A. Sass, MD, FACG2
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Stratford, NJ
Introduction: Fluid overload-associated large B cell lymphoma (FOA-LBCL) is a rare lymphoma presenting as an isolated effusion in body cavities without an associated tumor mass or lymphadenopathy. This entity is associated with volume-overloaded states such as cirrhosis. We report a unique case of a patient with Hepatitis C cirrhosis who presented with high leukocyte count in ascites initially concerning for spontaneous bacterial peritonitis (SBP) but later recognized as FOA-LBCL.
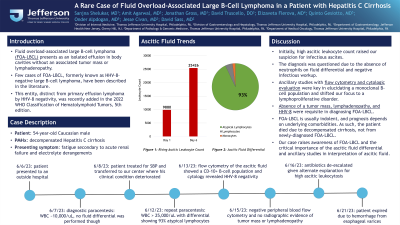
Case Description/Methods: A 54-year-old male with decompensated Hepatitis C cirrhosis with refractory ascites presented to an outside hospital with acute kidney injury and electrolyte derangements, requiring hemodialysis. At that time, diagnostic paracentesis was significant for elevated leukocyte count of just under 10,000/ μL. No differential was performed on that initial cell count though.
He was treated for SBP and transferred to our center, where his clinical condition worsened. CT scan of the abdomen showed no evidence of secondary bacterial peritonitis, and gram stain and culture of ascitic fluid were negative. Repeat paracentesis showed rising ascitic leukocyte count to over 25,000/μL, with differential showing 93% atypical lymphocytes. Flow cytometry of the ascitic fluid revealed a monoclonal CD10+ B-cell population. Further workup results included negative peripheral blood flow cytometry and no evidence of neck, thoracic, or intrabdominal masses or lymphadenopathy on CT imaging.
Given the constellation of a monoclonal CD10+ B-cell population restricted to ascitic fluid, lack of identifiable mass or lymphadenopathy, and history of cirrhosis, the overall findings were consistent with FOA-LBCL. Antibiotics were de-escalated given an alternative explanation for high ascitic leukocytosis and all culture data remaining negative. The patient died soon after due to a massive upper gastrointestinal hemorrhage from esophageal varices.
Discussion: FOA-LBCL, although rare, should be considered in patients with body cavity effusions with high leukocyte count which are refractory to antimicrobials. Ancillary studies with flow cytometry and cytologic evaluation of the ascitic fluid are essential in confirming the diagnosis of lymphoproliferative disease. Absence of an infectious source, extracavitary mass, and lymphadenopathy were also requisite for diagnosis. This case raises awareness of FOA-LBCL and highlights the importance of the ascitic leukocyte differential and ancillary studies in interpretation of ascites fluid analysis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sanjna Shelukar, MD1, Amit Agarwal, MD2, Jonathan Gross, MD2, David Truscello, DO3, Elizaveta Flerova, MD2, Quinto Gesiotto, MD2, Onder Alpdogan, MD2, Jesse M. Civan, MD2, David A. Sass, MD, FACG2. P1337 - A Rare Case of Fluid Overload-Associated Large B Cell Lymphoma in a Patient With Hepatitis C Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Stratford, NJ
Introduction: Fluid overload-associated large B cell lymphoma (FOA-LBCL) is a rare lymphoma presenting as an isolated effusion in body cavities without an associated tumor mass or lymphadenopathy. This entity is associated with volume-overloaded states such as cirrhosis. We report a unique case of a patient with Hepatitis C cirrhosis who presented with high leukocyte count in ascites initially concerning for spontaneous bacterial peritonitis (SBP) but later recognized as FOA-LBCL.
Case Description/Methods: A 54-year-old male with decompensated Hepatitis C cirrhosis with refractory ascites presented to an outside hospital with acute kidney injury and electrolyte derangements, requiring hemodialysis. At that time, diagnostic paracentesis was significant for elevated leukocyte count of just under 10,000/ μL. No differential was performed on that initial cell count though.
He was treated for SBP and transferred to our center, where his clinical condition worsened. CT scan of the abdomen showed no evidence of secondary bacterial peritonitis, and gram stain and culture of ascitic fluid were negative. Repeat paracentesis showed rising ascitic leukocyte count to over 25,000/μL, with differential showing 93% atypical lymphocytes. Flow cytometry of the ascitic fluid revealed a monoclonal CD10+ B-cell population. Further workup results included negative peripheral blood flow cytometry and no evidence of neck, thoracic, or intrabdominal masses or lymphadenopathy on CT imaging.
Given the constellation of a monoclonal CD10+ B-cell population restricted to ascitic fluid, lack of identifiable mass or lymphadenopathy, and history of cirrhosis, the overall findings were consistent with FOA-LBCL. Antibiotics were de-escalated given an alternative explanation for high ascitic leukocytosis and all culture data remaining negative. The patient died soon after due to a massive upper gastrointestinal hemorrhage from esophageal varices.
Discussion: FOA-LBCL, although rare, should be considered in patients with body cavity effusions with high leukocyte count which are refractory to antimicrobials. Ancillary studies with flow cytometry and cytologic evaluation of the ascitic fluid are essential in confirming the diagnosis of lymphoproliferative disease. Absence of an infectious source, extracavitary mass, and lymphadenopathy were also requisite for diagnosis. This case raises awareness of FOA-LBCL and highlights the importance of the ascitic leukocyte differential and ancillary studies in interpretation of ascites fluid analysis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sanjna Shelukar indicated no relevant financial relationships.
Amit Agarwal indicated no relevant financial relationships.
Jonathan Gross indicated no relevant financial relationships.
David Truscello indicated no relevant financial relationships.
Elizaveta Flerova indicated no relevant financial relationships.
Quinto Gesiotto indicated no relevant financial relationships.
Onder Alpdogan indicated no relevant financial relationships.
Jesse Civan indicated no relevant financial relationships.
David Sass indicated no relevant financial relationships.
Sanjna Shelukar, MD1, Amit Agarwal, MD2, Jonathan Gross, MD2, David Truscello, DO3, Elizaveta Flerova, MD2, Quinto Gesiotto, MD2, Onder Alpdogan, MD2, Jesse M. Civan, MD2, David A. Sass, MD, FACG2. P1337 - A Rare Case of Fluid Overload-Associated Large B Cell Lymphoma in a Patient With Hepatitis C Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
