Sunday Poster Session
Category: Liver
P1388 - Sequential AIH-PBC Overlap Syndrome: Decompensated Primary Biliary Cholangitis Secondary to De-Novo Autoimmune Hepatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Makeda Dawkins, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Makeda Dawkins, MD, Michael Rosman, MD, Roxana Bodin, MD
Westchester Medical Center, Valhalla, NY
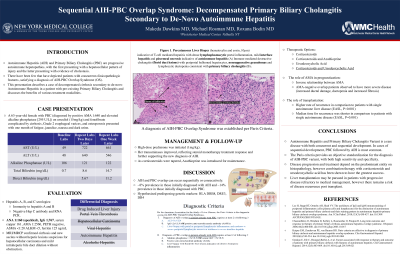
Introduction: Autoimmune Hepatitis (AIH) and Primary Biliary Cholangitis (PBC) are progressive autoimmune hepatopathies. Few cases have depicted patients with concurrent clinicopathologic features, satisfying a diagnosis of AIH-PBC Overlap Syndrome (OS). This presentation describes a case of decompensated cirrhosis secondary to de-novo Autoimmune Hepatitis in a patient with pre-existing Primary Biliary Cholangitis and discusses the benefits of various treatment modalities.
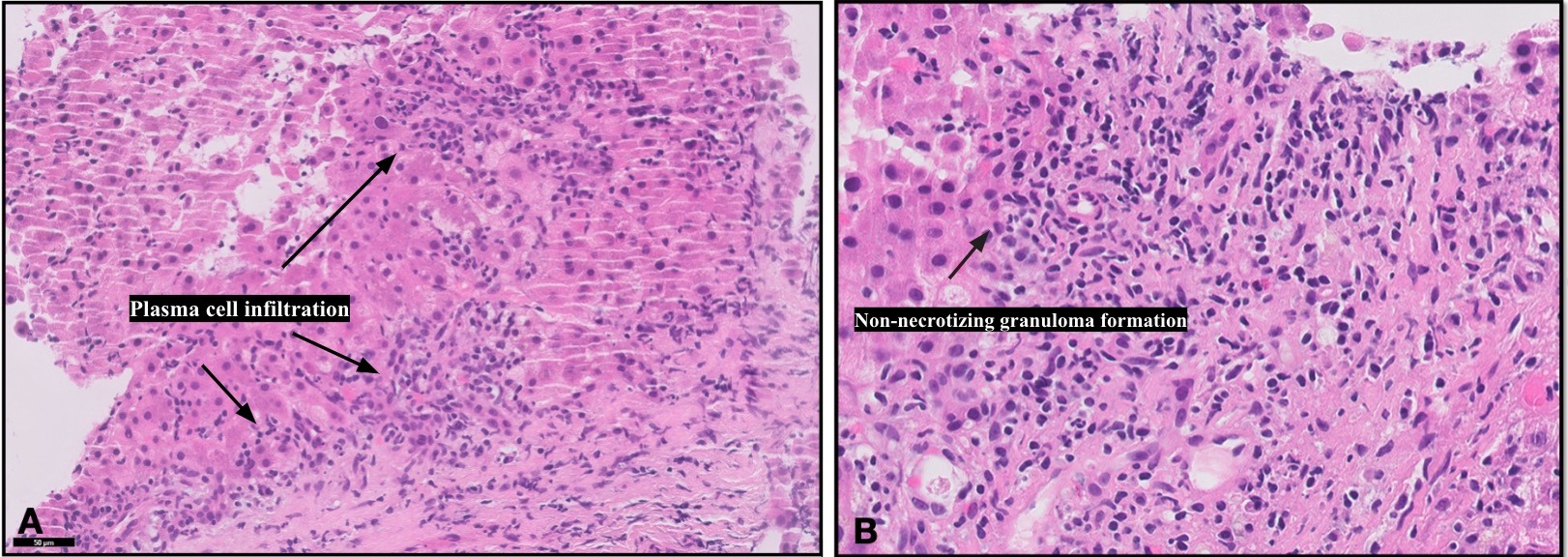
Case Description/Methods: A 63-year-old female with PBC complicated by cirrhosis, on ursodiol (15mg/kg), presented with one month of fatigue, jaundice, and dark urine, with transaminases >10x ULN, elevated alkaline phosphatase, and hyperbilirubinemia. Hepatitis A, B, and C serologies were negative for infection. MRI abdomen showed intrahepatic ductal dilation without extrahepatic abnormalities. Extended labs showed a newly positive antinuclear antibody and elevated IgG. Liver biopsy confirmed PBC by nonsuppurative granulation and interlobular bile duct destruction and noted new lymphoplasmacytic portal infiltration with moderate interface hepatitis suggestive of AIH. A diagnosis of Autoimmune Hepatitis-Primary Biliary Cirrhosis Overlap Syndrome was made per Paris Criteria. High-dose prednisone was initiated (1mg/kg). Her transaminases improved, reflecting steroid monotherapy treatment response and further supporting the new diagnosis of AIH. As corticosteroids were tapered, Azathioprine was introduced for remission maintenance.
Discussion: Although discussion is ongoing on whether overlap syndromes represent two distinct diseases in coexistence or atypical presentations of a singular entity, this case is a rare depiction of sequential AIH-PBC Overlap Syndrome. There are no known risk factors for AIH-PBC OS, however, hypothesized pathophysiologic mechanisms include shared IRF5, TNFRSF14, and SH2B3 pleomorphic genes and their roles in innate and adaptive immunity. The Paris Criteria remains the gold standard for diagnosis. Treatment is most successful in patients receiving combination corticosteroid-ursodiol therapy. Liver transplant may be pursued in refractory disease; albeit recurrence can occur in transplanted allografts. Small observational studies have reported worse outcomes in patients with AIH-PBC OS compared to those with AIH or PBC alone, including complications of portal hypertension, death, or need for liver transplant. This case highlights the need to consider overlap syndromes in patients with newly decompensated liver disease.
Disclosures:
Makeda Dawkins, MD, Michael Rosman, MD, Roxana Bodin, MD. P1388 - Sequential AIH-PBC Overlap Syndrome: Decompensated Primary Biliary Cholangitis Secondary to De-Novo Autoimmune Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Autoimmune Hepatitis (AIH) and Primary Biliary Cholangitis (PBC) are progressive autoimmune hepatopathies. Few cases have depicted patients with concurrent clinicopathologic features, satisfying a diagnosis of AIH-PBC Overlap Syndrome (OS). This presentation describes a case of decompensated cirrhosis secondary to de-novo Autoimmune Hepatitis in a patient with pre-existing Primary Biliary Cholangitis and discusses the benefits of various treatment modalities.
Case Description/Methods: A 63-year-old female with PBC complicated by cirrhosis, on ursodiol (15mg/kg), presented with one month of fatigue, jaundice, and dark urine, with transaminases >10x ULN, elevated alkaline phosphatase, and hyperbilirubinemia. Hepatitis A, B, and C serologies were negative for infection. MRI abdomen showed intrahepatic ductal dilation without extrahepatic abnormalities. Extended labs showed a newly positive antinuclear antibody and elevated IgG. Liver biopsy confirmed PBC by nonsuppurative granulation and interlobular bile duct destruction and noted new lymphoplasmacytic portal infiltration with moderate interface hepatitis suggestive of AIH. A diagnosis of Autoimmune Hepatitis-Primary Biliary Cirrhosis Overlap Syndrome was made per Paris Criteria. High-dose prednisone was initiated (1mg/kg). Her transaminases improved, reflecting steroid monotherapy treatment response and further supporting the new diagnosis of AIH. As corticosteroids were tapered, Azathioprine was introduced for remission maintenance.
Discussion: Although discussion is ongoing on whether overlap syndromes represent two distinct diseases in coexistence or atypical presentations of a singular entity, this case is a rare depiction of sequential AIH-PBC Overlap Syndrome. There are no known risk factors for AIH-PBC OS, however, hypothesized pathophysiologic mechanisms include shared IRF5, TNFRSF14, and SH2B3 pleomorphic genes and their roles in innate and adaptive immunity. The Paris Criteria remains the gold standard for diagnosis. Treatment is most successful in patients receiving combination corticosteroid-ursodiol therapy. Liver transplant may be pursued in refractory disease; albeit recurrence can occur in transplanted allografts. Small observational studies have reported worse outcomes in patients with AIH-PBC OS compared to those with AIH or PBC alone, including complications of portal hypertension, death, or need for liver transplant. This case highlights the need to consider overlap syndromes in patients with newly decompensated liver disease.
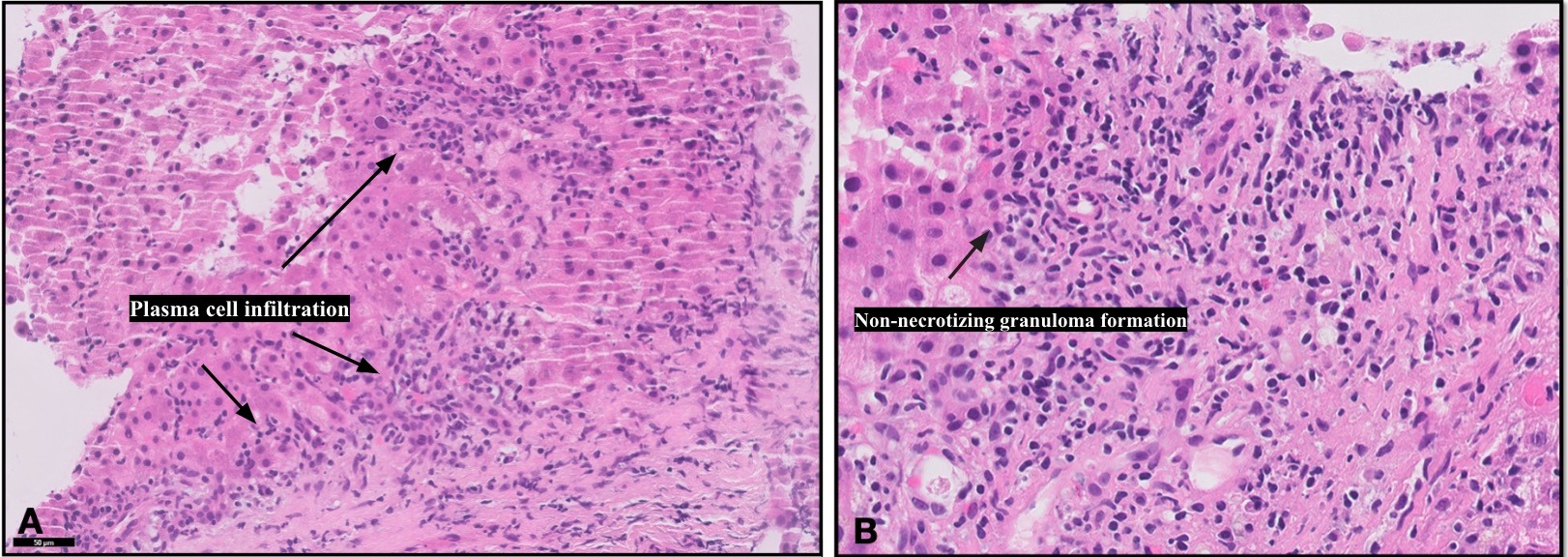
Figure: Figure 1: Liver Biopsy (hematoxylin and eosin, 10µm) with T-cell mediated hepatitis, dense lymphoplasmacytic portal inflammation, mild interface hepatitis and piecemeal necrosis indicative of autoimmune hepatitis (A) and immune-mediated destructive cholangitis (florid duct lesions) with periportal ballooned hepatocytes, nonsuppurative granulomas and lymphocytic ductopenia consistent with primary biliary cholangitis (B).
Disclosures:
Makeda Dawkins indicated no relevant financial relationships.
Michael Rosman indicated no relevant financial relationships.
Roxana Bodin indicated no relevant financial relationships.
Makeda Dawkins, MD, Michael Rosman, MD, Roxana Bodin, MD. P1388 - Sequential AIH-PBC Overlap Syndrome: Decompensated Primary Biliary Cholangitis Secondary to De-Novo Autoimmune Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

