Sunday Poster Session
Category: Liver
P1392 - Navigating Treatment Priorities: A Case of Concurrent Hepatocellular Carcinoma with Retroperitoneal Malignant Peripheral Nerve Sheath Tumor
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Anthony Quiej, BA
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Anthony Quiej, BA, Lindsay Thornton, MD, Nkiruka Ezenwajiaku, MD, Patricia Jones, MD, MSCR
University of Miami Miller School of Medicine, Miami, FL
Introduction: Hepatocellular carcinoma (HCC) can be diagnosed by multiphase imaging alone and is characterized by hyperenhancement in the arterial phase and washout in delayed phases. While HCC can metastasize to lymph nodes, lung, bone, and the adrenal glands, metastatic lesions in HCC are not routinely biopsied. We biopsied a lesion, presumed to be metastatic HCC and present a case of advanced hepatocellular carcinoma (HCC) diagnosed concurrently with retroperitoneal malignant peripheral nerve sheath tumor (MPNST). Treatment of multiple primary tumors requires prioritization of treatment and an interdisciplinary approach to patient management, to optimize patient outcomes.
Case Description/Methods: A 68 y.o. male without prior history of liver disease was referred to Hepatology for liver mass and elevated alpha-fetoprotein (AFP=10,643 ng/mL). Imaging was highly suspicious for hepatocellular carcinoma (HCC). He also had an 8 cm mass in the right adrenal gland, concerning for metastatic HCC. Biopsies of both masses were taken, pathology confirmed concurrent HCC and MPNST.
He was subsequently referred to Oncology, however, there is no treatment overlap for MPNST and HCC. He received concurrent treatment for his cancers. He received three cycles of Doxorubicin/Ifosfamide (DI) to target the MPNST and Y-90 for HCC. His initial treatment course was complicated by pancytopenia and gastrointestinal bleeding.
Interval imaging s/p systemic treatment and Y-90 showed stable to improved disease in both primary malignancies. AFP declined to 1,232 ng/mL. However, 3 months after Y-90, AFP rose and biopsy of lymph node confirmed HCC metastasis. Thus DI was held and Durvalumab was initiated. Imaging demonstrated stable liver lesions and stable to mild increase in the size of the adrenal mass. He received external beam radiation to the MPNST, followed by resection. The liver lesion enlarged and PET/CT showed more pronounced FDG avidity and new FDG avid mass. He received 10 cycles of Durvalumab with eventual progression of disease.
Discussion: Initial workup included biopsy of the adrenal mass to rule out metastatic HCC, which would impact eventual eligibility for transplant and shift treatment from locoregional to systemic. Although imaging and elevated AFP were highly suggestive of HCC, the adrenal mass was MPNST. Currently, there is no treatment overlap for MPNST and HCC. The diagnosis, treatment, and management of multiple primary tumors presents a challenge to clinicians.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anthony Quiej, BA, Lindsay Thornton, MD, Nkiruka Ezenwajiaku, MD, Patricia Jones, MD, MSCR. P1392 - Navigating Treatment Priorities: A Case of Concurrent Hepatocellular Carcinoma with Retroperitoneal Malignant Peripheral Nerve Sheath Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Miami Miller School of Medicine, Miami, FL
Introduction: Hepatocellular carcinoma (HCC) can be diagnosed by multiphase imaging alone and is characterized by hyperenhancement in the arterial phase and washout in delayed phases. While HCC can metastasize to lymph nodes, lung, bone, and the adrenal glands, metastatic lesions in HCC are not routinely biopsied. We biopsied a lesion, presumed to be metastatic HCC and present a case of advanced hepatocellular carcinoma (HCC) diagnosed concurrently with retroperitoneal malignant peripheral nerve sheath tumor (MPNST). Treatment of multiple primary tumors requires prioritization of treatment and an interdisciplinary approach to patient management, to optimize patient outcomes.
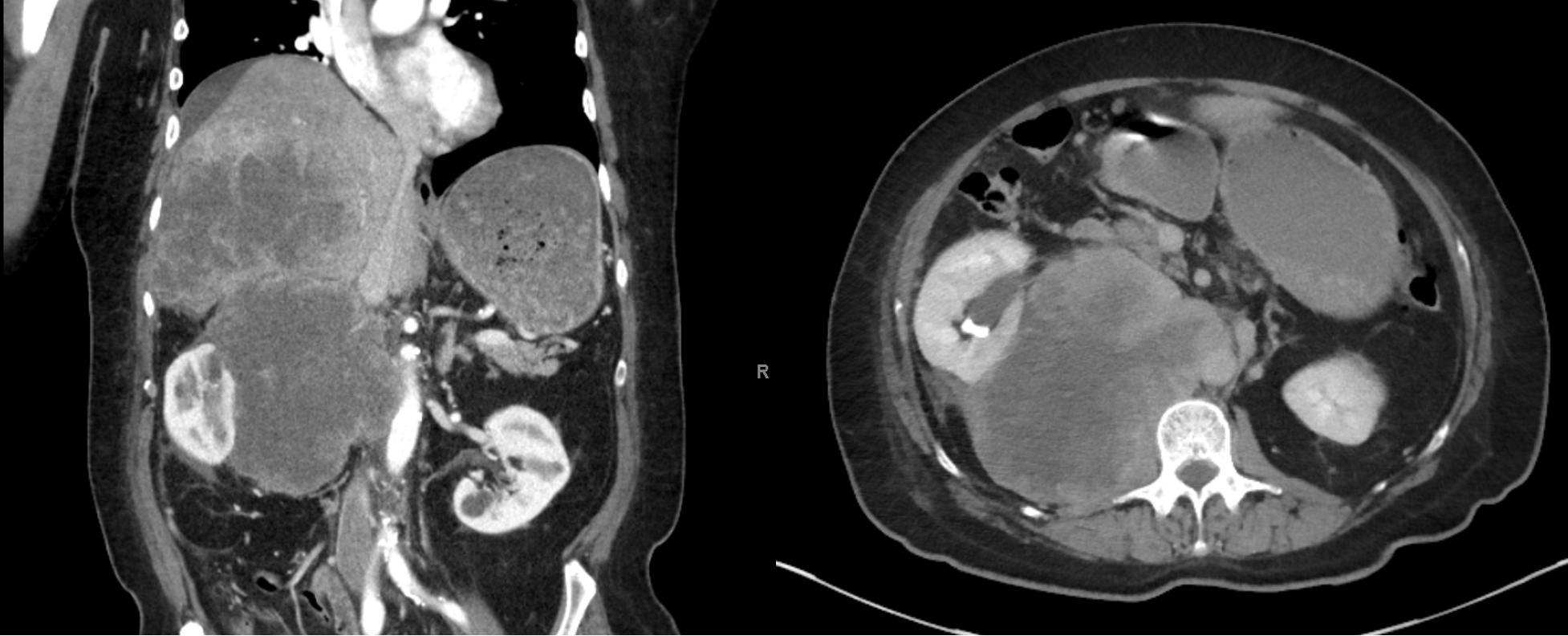
Case Description/Methods: A 68 y.o. male without prior history of liver disease was referred to Hepatology for liver mass and elevated alpha-fetoprotein (AFP=10,643 ng/mL). Imaging was highly suspicious for hepatocellular carcinoma (HCC). He also had an 8 cm mass in the right adrenal gland, concerning for metastatic HCC. Biopsies of both masses were taken, pathology confirmed concurrent HCC and MPNST.
He was subsequently referred to Oncology, however, there is no treatment overlap for MPNST and HCC. He received concurrent treatment for his cancers. He received three cycles of Doxorubicin/Ifosfamide (DI) to target the MPNST and Y-90 for HCC. His initial treatment course was complicated by pancytopenia and gastrointestinal bleeding.
Interval imaging s/p systemic treatment and Y-90 showed stable to improved disease in both primary malignancies. AFP declined to 1,232 ng/mL. However, 3 months after Y-90, AFP rose and biopsy of lymph node confirmed HCC metastasis. Thus DI was held and Durvalumab was initiated. Imaging demonstrated stable liver lesions and stable to mild increase in the size of the adrenal mass. He received external beam radiation to the MPNST, followed by resection. The liver lesion enlarged and PET/CT showed more pronounced FDG avidity and new FDG avid mass. He received 10 cycles of Durvalumab with eventual progression of disease.
Discussion: Initial workup included biopsy of the adrenal mass to rule out metastatic HCC, which would impact eventual eligibility for transplant and shift treatment from locoregional to systemic. Although imaging and elevated AFP were highly suggestive of HCC, the adrenal mass was MPNST. Currently, there is no treatment overlap for MPNST and HCC. The diagnosis, treatment, and management of multiple primary tumors presents a challenge to clinicians.
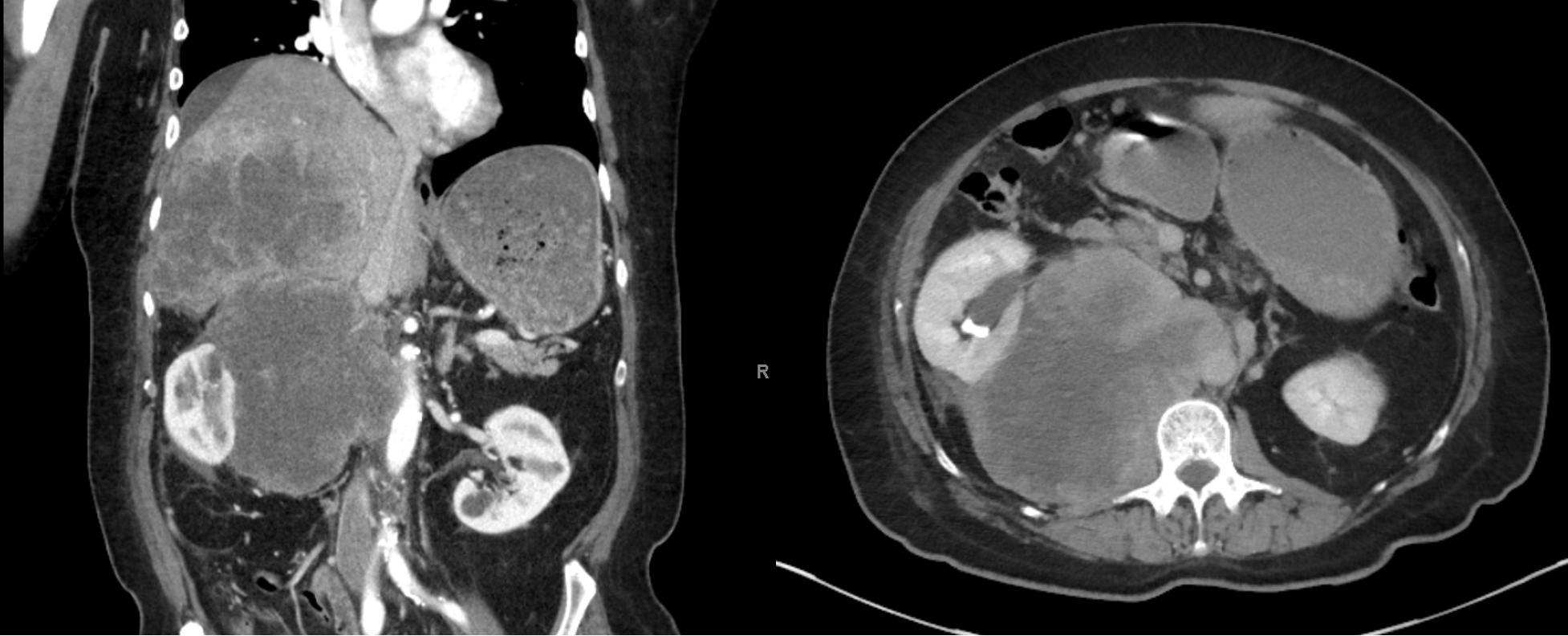
Figure: Post biopsy pre-treatment CT, December 2022. Imaging demonstrates rapid increase in size of the adrenal lesion.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anthony Quiej indicated no relevant financial relationships.
Lindsay Thornton indicated no relevant financial relationships.
Nkiruka Ezenwajiaku indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Anthony Quiej, BA, Lindsay Thornton, MD, Nkiruka Ezenwajiaku, MD, Patricia Jones, MD, MSCR. P1392 - Navigating Treatment Priorities: A Case of Concurrent Hepatocellular Carcinoma with Retroperitoneal Malignant Peripheral Nerve Sheath Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
