Sunday Poster Session
Category: Liver
P1398 - Autoimmune Hepatitis Masqueraded by Choledocholithiasis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Isabella Suarez Alcala, MD
Palmetto General Hospital
Hialeah, FL
Presenting Author(s)
Isabella Suarez Alcala, MD, Sebastian Hermida Velasquez, DO
Palmetto General Hospital, Hialeah, FL
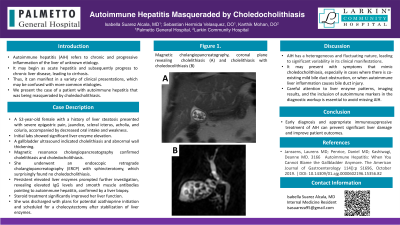
Introduction: Autoimmune hepatitis refers to chronic and progressive inflammation of the liver of unknown etiology. It may begin as acute hepatitis and subsequently progress to chronic liver disease, leading to cirrhosis. Thus, it can manifest in a variety of clinical presentations, which may be confused with more common etiologies. We present the case of a patient with autoimmune hepatitis that was being masqueraded by choledocholithiasis.
Case Description/Methods: A 52-year-old female with a history of liver steatosis presented with severe epigastric pain, jaundice, scleral icterus, acholia, and coluria, accompanied by decreased oral intake and weakness. Her initial labs showed significant liver enzyme elevation: AST at 1460 U/L, ALT at 1388 U/L, alkaline phosphatase at 190 U/L, and total bilirubin at 22.6 mg/dL. Abdominal CT scans revealed no acute abnormalities, but a gallbladder ultrasound indicated cholelithiasis and abnormal wall thickening. Magnetic resonance cholangiopancreatography confirmed cholelithiasis and choledocholithiasis. She underwent an endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy at a specialized center, which surprisingly found no choledocholithiasis. Persistent elevated liver enzymes prompted further investigation, ruling out acetaminophen toxicity, alcohol-related liver disease, and viral hepatitis. Elevated IgG levels and smooth muscle antibodies pointed to autoimmune hepatitis, confirmed by a liver biopsy showing moderate chronic portal lymphoplasmacytic inflammation, mixed acute and chronic lobular inflammation, mild to moderate fibrosis, and diffuse hepatocellular cholestasis. Steroid treatment significantly improved her liver function, leading to decreases in total bilirubin to 14.8 mg/dL, AST to 670 U/L, and ALT to 975 U/L. She was discharged for outpatient follow-up, with plans for potential azathioprine initiation depending on thiopurine methyltransferase levels and scheduled for a cholecystectomy after stabilization of liver enzymes.
Discussion: This case underscores the complexity of diagnosing autoimmune hepatitis, particularly when symptoms and initial findings suggest more common biliary disorders such as choledocholithiasis. Persistent elevations in liver enzymes despite biliary interventions prompted a deeper diagnostic evaluation, revealing autoimmune hepatitis. This illustrates the importance of considering autoimmune etiologies in patients with atypical liver profiles and highlights the effectiveness of tailored immunosuppressive therapy.
Disclosures:
Isabella Suarez Alcala, MD, Sebastian Hermida Velasquez, DO. P1398 - Autoimmune Hepatitis Masqueraded by Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Palmetto General Hospital, Hialeah, FL
Introduction: Autoimmune hepatitis refers to chronic and progressive inflammation of the liver of unknown etiology. It may begin as acute hepatitis and subsequently progress to chronic liver disease, leading to cirrhosis. Thus, it can manifest in a variety of clinical presentations, which may be confused with more common etiologies. We present the case of a patient with autoimmune hepatitis that was being masqueraded by choledocholithiasis.
Case Description/Methods: A 52-year-old female with a history of liver steatosis presented with severe epigastric pain, jaundice, scleral icterus, acholia, and coluria, accompanied by decreased oral intake and weakness. Her initial labs showed significant liver enzyme elevation: AST at 1460 U/L, ALT at 1388 U/L, alkaline phosphatase at 190 U/L, and total bilirubin at 22.6 mg/dL. Abdominal CT scans revealed no acute abnormalities, but a gallbladder ultrasound indicated cholelithiasis and abnormal wall thickening. Magnetic resonance cholangiopancreatography confirmed cholelithiasis and choledocholithiasis. She underwent an endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy at a specialized center, which surprisingly found no choledocholithiasis. Persistent elevated liver enzymes prompted further investigation, ruling out acetaminophen toxicity, alcohol-related liver disease, and viral hepatitis. Elevated IgG levels and smooth muscle antibodies pointed to autoimmune hepatitis, confirmed by a liver biopsy showing moderate chronic portal lymphoplasmacytic inflammation, mixed acute and chronic lobular inflammation, mild to moderate fibrosis, and diffuse hepatocellular cholestasis. Steroid treatment significantly improved her liver function, leading to decreases in total bilirubin to 14.8 mg/dL, AST to 670 U/L, and ALT to 975 U/L. She was discharged for outpatient follow-up, with plans for potential azathioprine initiation depending on thiopurine methyltransferase levels and scheduled for a cholecystectomy after stabilization of liver enzymes.
Discussion: This case underscores the complexity of diagnosing autoimmune hepatitis, particularly when symptoms and initial findings suggest more common biliary disorders such as choledocholithiasis. Persistent elevations in liver enzymes despite biliary interventions prompted a deeper diagnostic evaluation, revealing autoimmune hepatitis. This illustrates the importance of considering autoimmune etiologies in patients with atypical liver profiles and highlights the effectiveness of tailored immunosuppressive therapy.
Disclosures:
Isabella Suarez Alcala indicated no relevant financial relationships.
Sebastian Hermida Velasquez indicated no relevant financial relationships.
Isabella Suarez Alcala, MD, Sebastian Hermida Velasquez, DO. P1398 - Autoimmune Hepatitis Masqueraded by Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
