Sunday Poster Session
Category: Liver
P1400 - Oxaliplatin-Induced Non-Cirrhotic Portal Hypertension
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Joshua Freeman, DO
Swedish Covenant Hospital
Chicago, IL
Presenting Author(s)
Joshua Freeman, DO, Andrew Moore, MD
Swedish Covenant Hospital, Chicago, IL
Introduction: Oxaliplatin is a platinum-containing chemotherapeutic agent for the treatment of stage III and IV colorectal carcinoma that has been associated with non-cirrhotic portal hypertension (NCPH). NCPH has life-threatening consequences such as variceal bleeding. We report a case of variceal bleeding from NCPH that developed years after completion of oxaliplatin.
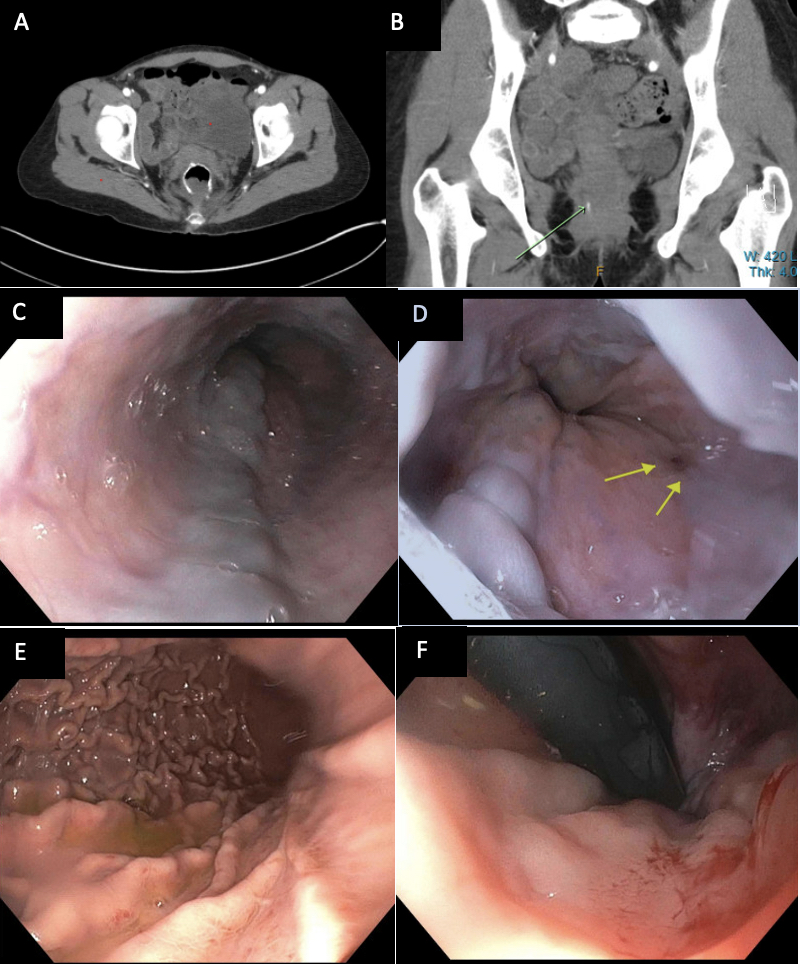
Case Description/Methods: 50 year old female with a history of metastatic rectal cancer treated with partial liver resection, radiation therapy and with 12 cycles of FOLFOXIRI, who presented to ED with hematochezia with clots. On presentation, vitals were unremarkable, labs significant for hemoglobin of 8.9 which dropped to 7.5 the next morning. CTA of the abdomen showed small amount of extravasation into the rectum and rectal varices. An upper endoscopy and flexible sigmoidoscopy were performed. Upper endoscopy showed 2 columns of large esophageal varices with red wale sign, which were banded with 4 bands. Moderate portal hypertensive gastropathy was seen as well. Flexible sigmoidoscopy showed rectal varices. She was started on PPI, octreotide drip, carvedilol twice daily and had IR guided liver biopsy. Biopsy showed no evidence of liver damage, but did show an elevated hepatic venous pressure gradient (HVPG) at 8mHg. Free hepatic vein measurement was 7mmHg and wedged hepatic vein was 15mmHg, indicative of NCPH.
Discussion: NCPH can mimic cirrhosis and cause life-threatening bleeds and should be identified quickly for proper treatment. In a multicenter retrospective study in Spain, they saw the prevalence of patients treated with oxaliplatin who developed NCPH to be about 0.5%. One proposed mechanism is via sinusoidal obstruction syndrome. Oxaliplatin induces direct damage on hepatic sinusoids, resulting in shedding of the endothelial lining. This leads to obstruction of the sinusoids and increases portal pressures. Biopsy needs to be done to rule out cirrhosis as the cause. Biopsy may reflect these changes; however, our patient had a normal liver biopsy which has been reported in other cases. Generally, esophageal/rectal varices appear with a HVPG > 12mmHg. Our patient's HVPG was 8mmHg, which we suspect to be due to her being on beta blocker at the time of liver biopsy. There are many disease states and medications that can lead to portal hypertension without cirrhosis, and it may even occur several years after discontinuation. Treatment is the same as for cirrhosis and may include TIPS procedure for refractory ascites/variceal bleeding.
Disclosures:
Joshua Freeman, DO, Andrew Moore, MD. P1400 - Oxaliplatin-Induced Non-Cirrhotic Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Swedish Covenant Hospital, Chicago, IL
Introduction: Oxaliplatin is a platinum-containing chemotherapeutic agent for the treatment of stage III and IV colorectal carcinoma that has been associated with non-cirrhotic portal hypertension (NCPH). NCPH has life-threatening consequences such as variceal bleeding. We report a case of variceal bleeding from NCPH that developed years after completion of oxaliplatin.
Case Description/Methods: 50 year old female with a history of metastatic rectal cancer treated with partial liver resection, radiation therapy and with 12 cycles of FOLFOXIRI, who presented to ED with hematochezia with clots. On presentation, vitals were unremarkable, labs significant for hemoglobin of 8.9 which dropped to 7.5 the next morning. CTA of the abdomen showed small amount of extravasation into the rectum and rectal varices. An upper endoscopy and flexible sigmoidoscopy were performed. Upper endoscopy showed 2 columns of large esophageal varices with red wale sign, which were banded with 4 bands. Moderate portal hypertensive gastropathy was seen as well. Flexible sigmoidoscopy showed rectal varices. She was started on PPI, octreotide drip, carvedilol twice daily and had IR guided liver biopsy. Biopsy showed no evidence of liver damage, but did show an elevated hepatic venous pressure gradient (HVPG) at 8mHg. Free hepatic vein measurement was 7mmHg and wedged hepatic vein was 15mmHg, indicative of NCPH.
Discussion: NCPH can mimic cirrhosis and cause life-threatening bleeds and should be identified quickly for proper treatment. In a multicenter retrospective study in Spain, they saw the prevalence of patients treated with oxaliplatin who developed NCPH to be about 0.5%. One proposed mechanism is via sinusoidal obstruction syndrome. Oxaliplatin induces direct damage on hepatic sinusoids, resulting in shedding of the endothelial lining. This leads to obstruction of the sinusoids and increases portal pressures. Biopsy needs to be done to rule out cirrhosis as the cause. Biopsy may reflect these changes; however, our patient had a normal liver biopsy which has been reported in other cases. Generally, esophageal/rectal varices appear with a HVPG > 12mmHg. Our patient's HVPG was 8mmHg, which we suspect to be due to her being on beta blocker at the time of liver biopsy. There are many disease states and medications that can lead to portal hypertension without cirrhosis, and it may even occur several years after discontinuation. Treatment is the same as for cirrhosis and may include TIPS procedure for refractory ascites/variceal bleeding.
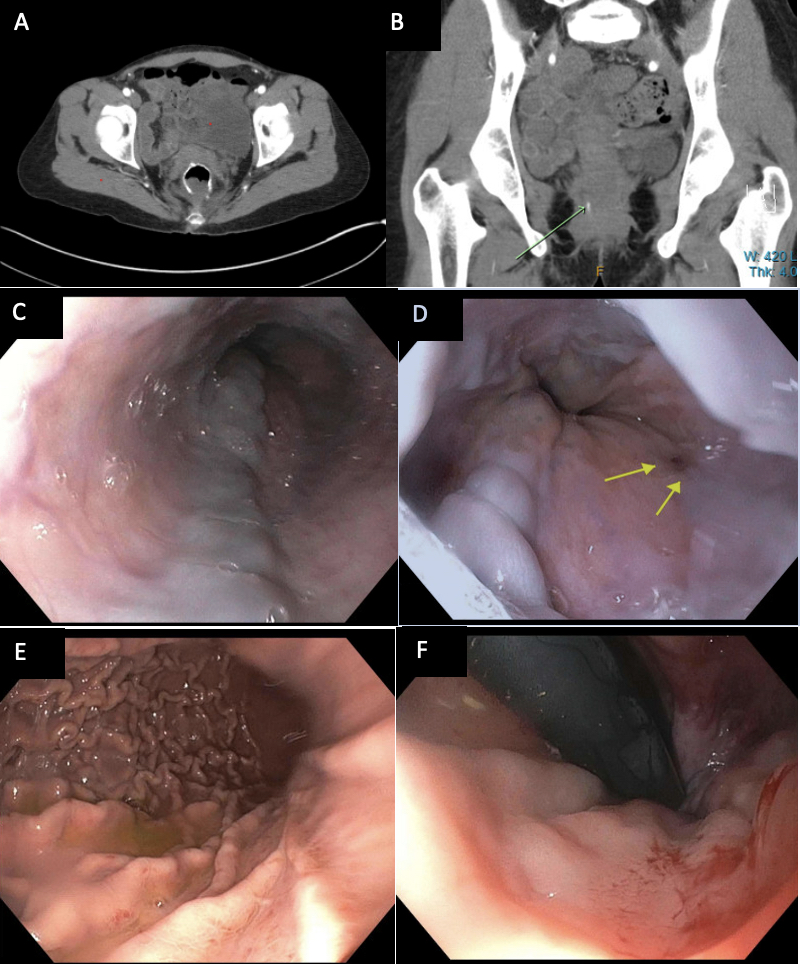
Figure: Figures A & B. CTA showing rectal varices with extravasation
Figures C & D. Esophageal varices, with red wale sign present
Figure E. Evidence of portal hypertensive gastropathy
Figure F. Rectal varices on flexible sigmoidoscopy
Figures C & D. Esophageal varices, with red wale sign present
Figure E. Evidence of portal hypertensive gastropathy
Figure F. Rectal varices on flexible sigmoidoscopy
Disclosures:
Joshua Freeman indicated no relevant financial relationships.
Andrew Moore indicated no relevant financial relationships.
Joshua Freeman, DO, Andrew Moore, MD. P1400 - Oxaliplatin-Induced Non-Cirrhotic Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
