Sunday Poster Session
Category: Liver
P1402 - Complications Associated With Intraperitoneal Fibrinolytic Therapy in Decompensated Cirrhosis Complicated by Infected Loculated Ascites
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Madeleine Z. Wong, MD
Stony Brook University Hospital
Central Islip, NY
Presenting Author(s)
Madeleine Z. Wong, MD1, Viraj Modi, DO2
1Stony Brook University Hospital, Central Islip, NY; 2Northport VA Medical Center, East Setauket, NY
Introduction: Spontaneous bacterial peritonitis (SBP) complicated by loculated ascites is rare in cirrhosis and presents as a challenge for many clinicians. The loculation of ascites limits percutaneous paracentesis, and poor penetration of antibiotics across sequestered bacterial fluid prevents adequate source control. To this date, treatment for loculated ascites in cirrhosis has not yet been established, however three cases successfully using intraperitoneal fibrinolytic therapy have been reported. We describe a case of unique complications from this novel treatment.
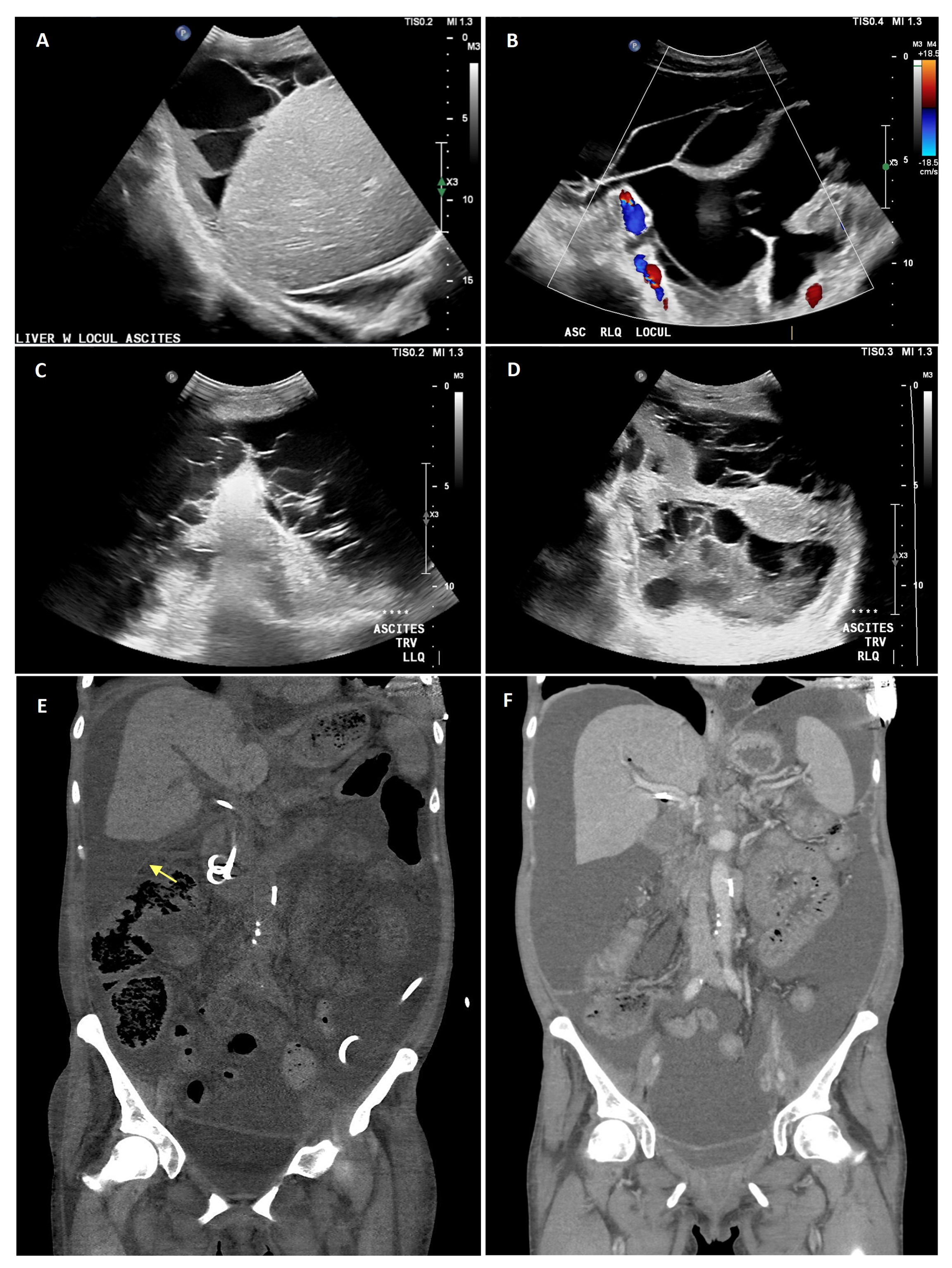
Case Description/Methods: A 59-year-old female with decompensated alcoholic cirrhosis and newly diagnosed pancreatic adenocarcinoma presented with multiple hospitalizations for recurrent SBP despite escalation of antibiotics. Ultrasound discovered large volume complex loculated ascites (fig. A & B). We attempted to mechanically break down the fibrins via wire during placement of a percutaneous pigtail drain. Tissue plasminogen activator (tPA) was also infused via the catheter with intent to chemically disrupt the loculations. Ascitic fluid drained post-tPA was notably more purulent than prior samples and imaging showed reduced volume loculations (fig. C & D). The patient however developed septic shock with hepatorenal syndrome, likely due to the release of viable bacteria from the dis-loculated ascites. We held further tPA treatments and the patient’s leukocytosis and renal function recovered over a week. Drainage from her catheter no longer met the criteria for SBP. New imaging, however, was apparent for a perihepatic loculation with new metastatic lesions in the liver (fig. E & F). Given the patient’s poor prognosis and aggressive nature of her cancer, the patient ultimately transitioned to comfort care.
Discussion: Loculated ascites have been associated with conditions that create hypo-fibrinolytic environments, such as malignancy. We demonstrated resolution of SBP with tPA infusions, however its treatment course was limited by an unexpected adverse reaction to it. Our imaging suggests that either one session of tPA infusion was not enough to relieve the peri-hepatic loculation, or the location of the catheter was incompatible. Additional tPA sessions were held in concern for causing further sepsis in an already frail patient, and the risk of hepatic bleeding in setting of new metastatic liver lesions. These unique complications are not discussed in literature but should be considered when weighing risks and limitations of this treatment.
Disclosures:
Madeleine Z. Wong, MD1, Viraj Modi, DO2. P1402 - Complications Associated With Intraperitoneal Fibrinolytic Therapy in Decompensated Cirrhosis Complicated by Infected Loculated Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Stony Brook University Hospital, Central Islip, NY; 2Northport VA Medical Center, East Setauket, NY
Introduction: Spontaneous bacterial peritonitis (SBP) complicated by loculated ascites is rare in cirrhosis and presents as a challenge for many clinicians. The loculation of ascites limits percutaneous paracentesis, and poor penetration of antibiotics across sequestered bacterial fluid prevents adequate source control. To this date, treatment for loculated ascites in cirrhosis has not yet been established, however three cases successfully using intraperitoneal fibrinolytic therapy have been reported. We describe a case of unique complications from this novel treatment.
Case Description/Methods: A 59-year-old female with decompensated alcoholic cirrhosis and newly diagnosed pancreatic adenocarcinoma presented with multiple hospitalizations for recurrent SBP despite escalation of antibiotics. Ultrasound discovered large volume complex loculated ascites (fig. A & B). We attempted to mechanically break down the fibrins via wire during placement of a percutaneous pigtail drain. Tissue plasminogen activator (tPA) was also infused via the catheter with intent to chemically disrupt the loculations. Ascitic fluid drained post-tPA was notably more purulent than prior samples and imaging showed reduced volume loculations (fig. C & D). The patient however developed septic shock with hepatorenal syndrome, likely due to the release of viable bacteria from the dis-loculated ascites. We held further tPA treatments and the patient’s leukocytosis and renal function recovered over a week. Drainage from her catheter no longer met the criteria for SBP. New imaging, however, was apparent for a perihepatic loculation with new metastatic lesions in the liver (fig. E & F). Given the patient’s poor prognosis and aggressive nature of her cancer, the patient ultimately transitioned to comfort care.
Discussion: Loculated ascites have been associated with conditions that create hypo-fibrinolytic environments, such as malignancy. We demonstrated resolution of SBP with tPA infusions, however its treatment course was limited by an unexpected adverse reaction to it. Our imaging suggests that either one session of tPA infusion was not enough to relieve the peri-hepatic loculation, or the location of the catheter was incompatible. Additional tPA sessions were held in concern for causing further sepsis in an already frail patient, and the risk of hepatic bleeding in setting of new metastatic liver lesions. These unique complications are not discussed in literature but should be considered when weighing risks and limitations of this treatment.
Figure: Abdominal Ultrasound showing large volume loculated ascites peri-hepatic (A) and in the RLQ (B) prior to fibrinolytic therapy. Abdominal Ultrasound showing moderate volume loculated ascites in the LLQ (C) and in the RLQ (D) post-fibrinolytic therapy. Non-contrasted computed tomography of the abdomen revealing a loculation of perihepatic ascites measuring 14.6 x 6.8 cm (yellow arrow) post-fibrinolytic therapy (E). Contrasted computed tomography of the abdomen prior to fibrinolytic therapy showing large volume ascites in the abdomen for comparison (F).
Disclosures:
Madeleine Wong indicated no relevant financial relationships.
Viraj Modi indicated no relevant financial relationships.
Madeleine Z. Wong, MD1, Viraj Modi, DO2. P1402 - Complications Associated With Intraperitoneal Fibrinolytic Therapy in Decompensated Cirrhosis Complicated by Infected Loculated Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
