Sunday Poster Session
Category: Liver
P1421 - Importance of Early Recognition and Treatment of Impending Umbilical Hernia Rupture
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Ixel Cervera, MD
NYU Langone Health
Brooklyn, NY
Presenting Author(s)
Ixel Cervera, MD, Saikiran Kilaru, MD
NYU Langone Health, New York, NY
Introduction: Flood syndrome is caused by spontaneous rupture of an umbilical hernia in the setting of long-standing ascites. It is a rare complication of end stage liver disease (ESLD). It is associated with high morbidity and mortality.
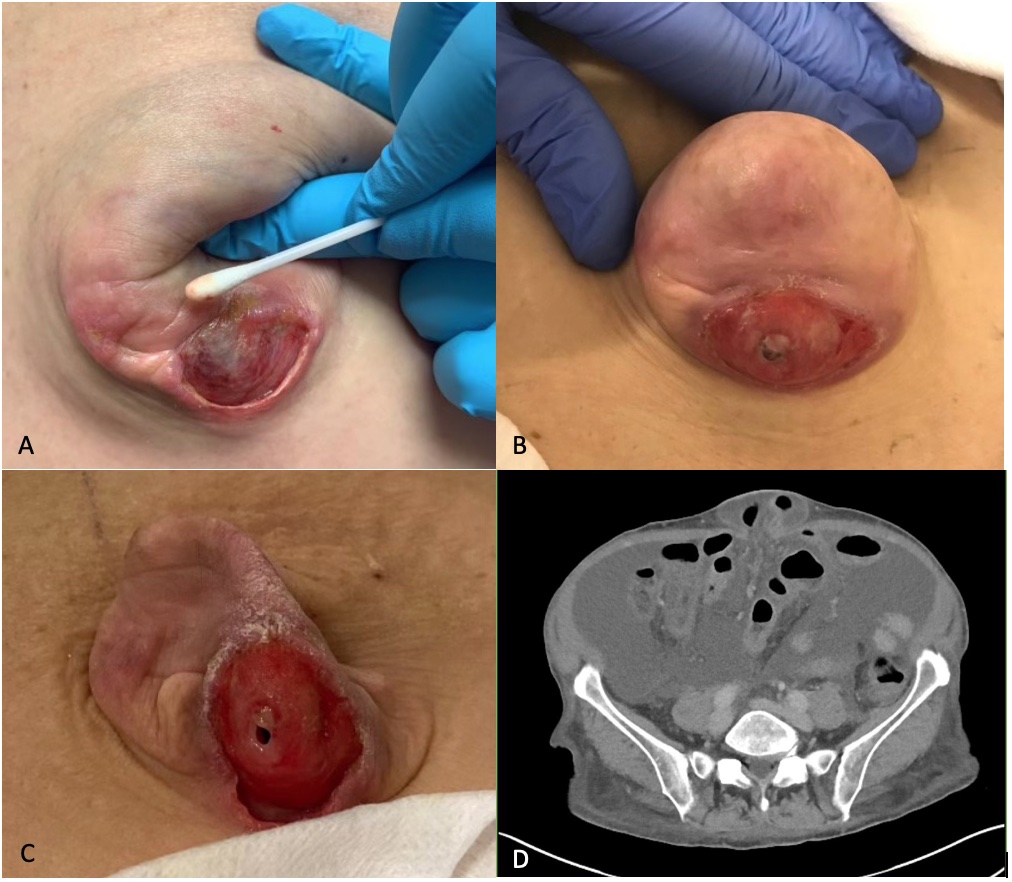
Case Description/Methods: A 58-year-old woman with history of alcohol use disorder complicated by ESLD with ascites developed an ulcerated umbilical hernia. She presented to the ED for fever, Tmax 100.9F. She had large volume paracentesis two days prior. In the ED she was afebrile HR 79 RR 16 BP 125/71. Physical exam showed a woman with a nontender protuberant soft abdomen with a large reducible hernia. Labs showed WBC 6.6, Hgb 10.9, Plt 155, Na 131, BUN 18, Cr 0.82, total bilirubin 5.6, normal transaminases, serum albumin 3.3. MELD-Na 22 up from baseline 14. Diagnostic paracentesis was negative for spontaneous bacterial peritonitis (SBP). CT abdomen pelvis (CTAP) was notable for omental haziness and thickened pelvic peritoneum concerning for peritonitis. The following day she began leaking clear fluid from the hernia with associated abdominal pain and cramping. She underwent an urgent open umbilical hernia repair with mesh with drain placement for ascites management. Her daily diuretics were resumed. She received a 7 day course of prophylactic cephalosporin. She was discharged on post-operative day 4. She was readmitted 3 weeks later with SBP (8474 PMNs), WBC 32, Na 109, BUN 79, Cr 3.5, Tbili 3.2, INR 1.3, MELD-Na 32. Fluid culture grew pan-sensitive Staph aureus. She was treated with piperacillin-tazobactam and micafungin. It was broadened to meropenem and oxacillin due to persistent ascites with >8000 PMNs. She received weeks of antibiotics with no improvement. CTAP did not show intrabdominal abscess. Blood cultures remained negative. She developed worsening AKI, and sepsis. Patient and family elected to convert to hospice, and patient perished.
Discussion: There are no specific guidelines for management of Flood syndrome. Conservative management focuses on local wound care, closure of skin defect with skin glue, while surgical management repairs hernia. Both focus on management of ascitic fluid and antibiotics to prevent peritonitis. Poor control results in 75% recurrence of hernia, peritonitis, and occasionally bowel obstruction and/or incarceration. Definitive surgical management is not without risks. The use of mesh for hernia repair reduces risk of recurrent hernia. Urgent surgical repair has higher morbidity and mortality than elective preventative repair.
Disclosures:
Ixel Cervera, MD, Saikiran Kilaru, MD. P1421 - Importance of Early Recognition and Treatment of Impending Umbilical Hernia Rupture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYU Langone Health, New York, NY
Introduction: Flood syndrome is caused by spontaneous rupture of an umbilical hernia in the setting of long-standing ascites. It is a rare complication of end stage liver disease (ESLD). It is associated with high morbidity and mortality.
Case Description/Methods: A 58-year-old woman with history of alcohol use disorder complicated by ESLD with ascites developed an ulcerated umbilical hernia. She presented to the ED for fever, Tmax 100.9F. She had large volume paracentesis two days prior. In the ED she was afebrile HR 79 RR 16 BP 125/71. Physical exam showed a woman with a nontender protuberant soft abdomen with a large reducible hernia. Labs showed WBC 6.6, Hgb 10.9, Plt 155, Na 131, BUN 18, Cr 0.82, total bilirubin 5.6, normal transaminases, serum albumin 3.3. MELD-Na 22 up from baseline 14. Diagnostic paracentesis was negative for spontaneous bacterial peritonitis (SBP). CT abdomen pelvis (CTAP) was notable for omental haziness and thickened pelvic peritoneum concerning for peritonitis. The following day she began leaking clear fluid from the hernia with associated abdominal pain and cramping. She underwent an urgent open umbilical hernia repair with mesh with drain placement for ascites management. Her daily diuretics were resumed. She received a 7 day course of prophylactic cephalosporin. She was discharged on post-operative day 4. She was readmitted 3 weeks later with SBP (8474 PMNs), WBC 32, Na 109, BUN 79, Cr 3.5, Tbili 3.2, INR 1.3, MELD-Na 32. Fluid culture grew pan-sensitive Staph aureus. She was treated with piperacillin-tazobactam and micafungin. It was broadened to meropenem and oxacillin due to persistent ascites with >8000 PMNs. She received weeks of antibiotics with no improvement. CTAP did not show intrabdominal abscess. Blood cultures remained negative. She developed worsening AKI, and sepsis. Patient and family elected to convert to hospice, and patient perished.
Discussion: There are no specific guidelines for management of Flood syndrome. Conservative management focuses on local wound care, closure of skin defect with skin glue, while surgical management repairs hernia. Both focus on management of ascitic fluid and antibiotics to prevent peritonitis. Poor control results in 75% recurrence of hernia, peritonitis, and occasionally bowel obstruction and/or incarceration. Definitive surgical management is not without risks. The use of mesh for hernia repair reduces risk of recurrent hernia. Urgent surgical repair has higher morbidity and mortality than elective preventative repair.
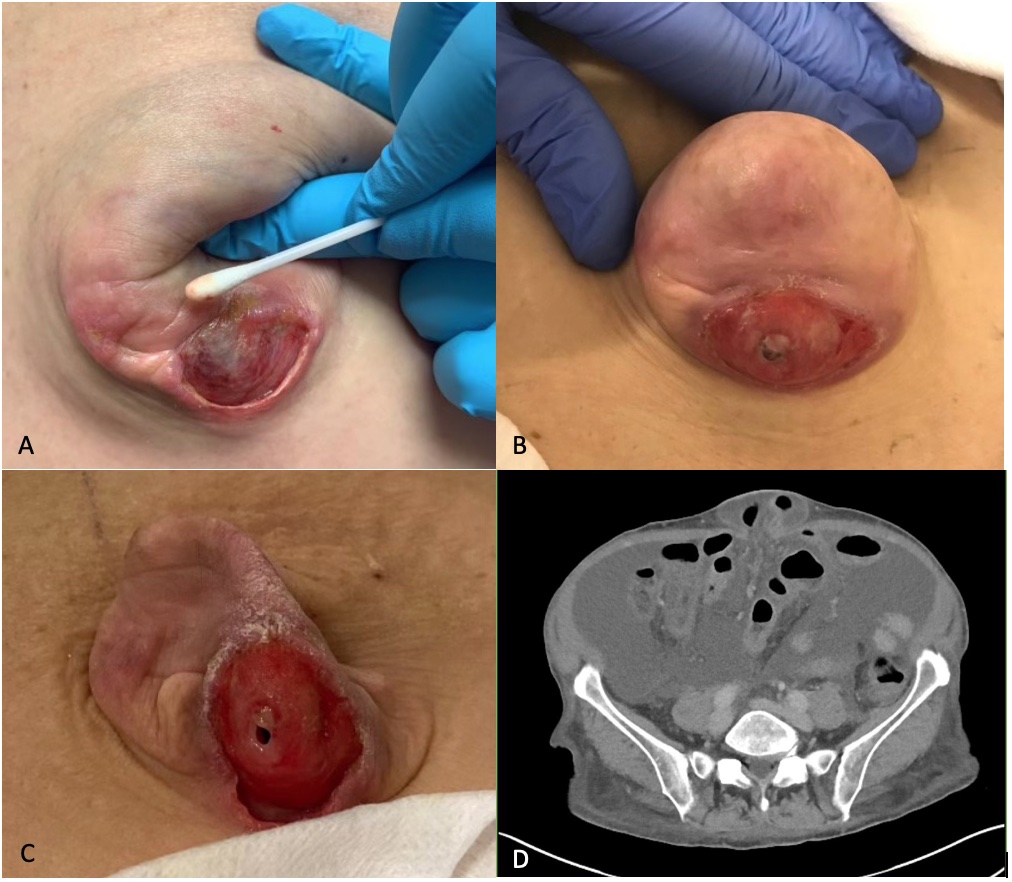
Figure: A. Ulcerated umbilical hernia noted in clinic. B. Umbilical hernia about to rupture. C. Umbilical hernia after rupture. D. CT AP showing unobstructed bowel in the hernia sac.
Disclosures:
Ixel Cervera indicated no relevant financial relationships.
Saikiran Kilaru indicated no relevant financial relationships.
Ixel Cervera, MD, Saikiran Kilaru, MD. P1421 - Importance of Early Recognition and Treatment of Impending Umbilical Hernia Rupture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
