Sunday Poster Session
Category: Liver
P1423 - A Case of Isolated Hepatic Artery Thrombosis in a Non-Transplant Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SO
Sean Olson, DO
University of Florida
Gainesville, FL
Presenting Author(s)
Sean Olson, DO, Kristin Price, MD
University of Florida, Gainesville, FL
Introduction: Hepatic artery thrombosis (HAT) is a rare entity most frequently associated with orthotopic liver transplantation (OLT) but has been reported in a few cases as an isolated phenomenon in patients who have not undergone OLT. In this case we will discuss isolated HAT as a rare cause of abdominal pain in a patient without a history of OLT.
Case Description/Methods: A 67-year-old female with a history of HTN, HLD, GERD, and surgical menopause who presented to the clinic for evaluation of abdominal pain. Ten days before her evaluation in the clinic, the patient experienced diarrhea overnight followed by abdominal pain the following morning. The pain began in the epigastrium and then progressed to RUQ pain with radiation to the mid-thoracic region. The pain continued to progress for a week and was associated with severe anorexia and night sweats. At this time, the patient presented to her local ED. She was found to have mild gallbladder wall thickening on RUQ US and was discharged to home.
She continued to experience severe pain and anorexia and presented to the clinic several days later for further evaluation. At the time of evaluation in the clinic, the patient was in distress with severe pain, BP 170/91, and sitting in a tripod position. A CMP and CBC were obtained which were within normal limits. Given the duration and severity of the patient's abdominal pain and lack of appetite, she was recommended to return to the ED.
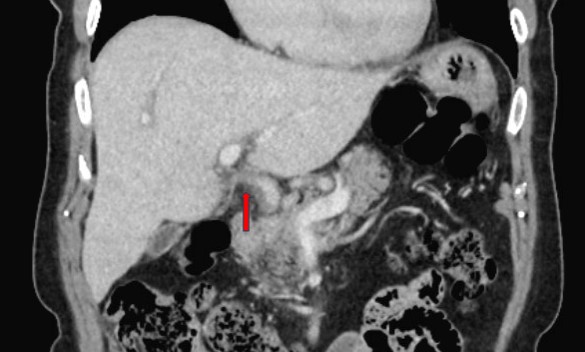
Evaluation in the ED included a CT A&P with IV contrast which revealed HAT. The patient was admitted to the hospital for pain control, IV hydration, anticoagulation, vascular surgery consultation, and hypercoagulability workup to further evaluate the etiology of her HAT. Given her lack of liver injury and incomplete occlusion of the hepatic artery, vascular intervention was deferred. Three-phase liver CT obtained the following day demonstrated stenosis of the common hepatic artery without definitive occlusive HAT. Her abdominal pain resolved, and she was able to tolerate food without nausea or vomiting. Hypercoagulable and malignancy workups were unrevealing. She was discharged home with instructions to start taking apixaban daily and withhold the use of estradiol.
Discussion: HAT is a rare cause of abdominal pain in patients without history of OLT and may present without laboratory evidence of liver injury. After a thorough workup for abdominal pain has been completed and the diagnosis is unclear, arterial phased cross-sectional imaging can be considered to rule out HAT.
Disclosures:
Sean Olson, DO, Kristin Price, MD. P1423 - A Case of Isolated Hepatic Artery Thrombosis in a Non-Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Florida, Gainesville, FL
Introduction: Hepatic artery thrombosis (HAT) is a rare entity most frequently associated with orthotopic liver transplantation (OLT) but has been reported in a few cases as an isolated phenomenon in patients who have not undergone OLT. In this case we will discuss isolated HAT as a rare cause of abdominal pain in a patient without a history of OLT.
Case Description/Methods: A 67-year-old female with a history of HTN, HLD, GERD, and surgical menopause who presented to the clinic for evaluation of abdominal pain. Ten days before her evaluation in the clinic, the patient experienced diarrhea overnight followed by abdominal pain the following morning. The pain began in the epigastrium and then progressed to RUQ pain with radiation to the mid-thoracic region. The pain continued to progress for a week and was associated with severe anorexia and night sweats. At this time, the patient presented to her local ED. She was found to have mild gallbladder wall thickening on RUQ US and was discharged to home.
She continued to experience severe pain and anorexia and presented to the clinic several days later for further evaluation. At the time of evaluation in the clinic, the patient was in distress with severe pain, BP 170/91, and sitting in a tripod position. A CMP and CBC were obtained which were within normal limits. Given the duration and severity of the patient's abdominal pain and lack of appetite, she was recommended to return to the ED.
Evaluation in the ED included a CT A&P with IV contrast which revealed HAT. The patient was admitted to the hospital for pain control, IV hydration, anticoagulation, vascular surgery consultation, and hypercoagulability workup to further evaluate the etiology of her HAT. Given her lack of liver injury and incomplete occlusion of the hepatic artery, vascular intervention was deferred. Three-phase liver CT obtained the following day demonstrated stenosis of the common hepatic artery without definitive occlusive HAT. Her abdominal pain resolved, and she was able to tolerate food without nausea or vomiting. Hypercoagulable and malignancy workups were unrevealing. She was discharged home with instructions to start taking apixaban daily and withhold the use of estradiol.
Discussion: HAT is a rare cause of abdominal pain in patients without history of OLT and may present without laboratory evidence of liver injury. After a thorough workup for abdominal pain has been completed and the diagnosis is unclear, arterial phased cross-sectional imaging can be considered to rule out HAT.
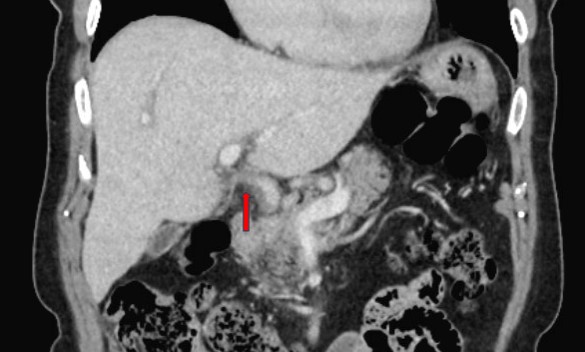
Figure: Figure 1. Enlargement of the distal common hepatic artery and possibly the proximal proper hepatic artery, with abrupt transition to a poorly opacified remaining portion of the proper hepatic artery which is consistent with hepatic artery thrombosis.
Disclosures:
Sean Olson indicated no relevant financial relationships.
Kristin Price indicated no relevant financial relationships.
Sean Olson, DO, Kristin Price, MD. P1423 - A Case of Isolated Hepatic Artery Thrombosis in a Non-Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
