Sunday Poster Session
Category: Obesity
P1457 - Intragastric Balloon-Induced Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Mina Fransawy Alkomos, MD
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Mina Alkomos, MD1, Alisa Farokhian, MD1, Nagihan Orhun, MD1, Furqan Bhullar, MD1, Nida Ansari, MD1, Nader Mekheal, MD1, Beshoy Effat Elkomos, MD2, Yana Cavanagh, MD1, Walid Baddoura, MD1, Kamal Amer, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2London North West University Healthcare, London, England, United Kingdom
Introduction: The intragastric balloon has been used for weight loss with approximately 10% to 15% total body weight loss over a 6-month period. It has a wide range of adverse effects, ranging from minor side effects such as Nausea, abdominal pain, and reflux to more serious complications such as intestinal obstruction, ulceration, perforation, and rare cases of acute pancreatitis.
Case Description/Methods: A 32-year male with a history of morbid obesity status post gastric balloon placement 18 months prior to his presentation to the emergency department for 2 weeks onset of worsening epigastric abdominal pain with nausea and vomiting. He relocated to the USA and did not have the chance to follow up for gastric balloon removal. He denies alcohol usage, and Labs were significant for elevated lipase of 1135, and Alkaline phosphatase of 109, otherwise unremarkable labs including CBC, CMP, and lipid panel. The CT abdomen/pelvis showed fat stranding and free fluid around the tail of the pancreas, a distended stomach with an intragastric balloon, and no signs of intestinal obstruction (Figure 1); the patient was diagnosed with intragastric balloon-induced pancreatitis and underwent successful resuscitation along with endoscopic gastric balloon removal (Figure 1).
Discussion: Few theories are described in the literature for the mechanism of this complication, including stomach overdistention with pancreatic compression at the tail or body or ampulla obstruction secondary to balloon migration at the duodenum. Those complications usually happen after 4-6 months, given balloon overdistention by time; however, it has also been reported earlier than 4 months. Reporting and Increasing physician awareness of this complication is important as the symptoms can be mistaken for balloon-related gastric abdominal pain, and a high index of suspicion is warranted for early diagnosis and management.
Disclosures:
Mina Alkomos, MD1, Alisa Farokhian, MD1, Nagihan Orhun, MD1, Furqan Bhullar, MD1, Nida Ansari, MD1, Nader Mekheal, MD1, Beshoy Effat Elkomos, MD2, Yana Cavanagh, MD1, Walid Baddoura, MD1, Kamal Amer, MD1. P1457 - Intragastric Balloon-Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2London North West University Healthcare, London, England, United Kingdom
Introduction: The intragastric balloon has been used for weight loss with approximately 10% to 15% total body weight loss over a 6-month period. It has a wide range of adverse effects, ranging from minor side effects such as Nausea, abdominal pain, and reflux to more serious complications such as intestinal obstruction, ulceration, perforation, and rare cases of acute pancreatitis.
Case Description/Methods: A 32-year male with a history of morbid obesity status post gastric balloon placement 18 months prior to his presentation to the emergency department for 2 weeks onset of worsening epigastric abdominal pain with nausea and vomiting. He relocated to the USA and did not have the chance to follow up for gastric balloon removal. He denies alcohol usage, and Labs were significant for elevated lipase of 1135, and Alkaline phosphatase of 109, otherwise unremarkable labs including CBC, CMP, and lipid panel. The CT abdomen/pelvis showed fat stranding and free fluid around the tail of the pancreas, a distended stomach with an intragastric balloon, and no signs of intestinal obstruction (Figure 1); the patient was diagnosed with intragastric balloon-induced pancreatitis and underwent successful resuscitation along with endoscopic gastric balloon removal (Figure 1).
Discussion: Few theories are described in the literature for the mechanism of this complication, including stomach overdistention with pancreatic compression at the tail or body or ampulla obstruction secondary to balloon migration at the duodenum. Those complications usually happen after 4-6 months, given balloon overdistention by time; however, it has also been reported earlier than 4 months. Reporting and Increasing physician awareness of this complication is important as the symptoms can be mistaken for balloon-related gastric abdominal pain, and a high index of suspicion is warranted for early diagnosis and management.
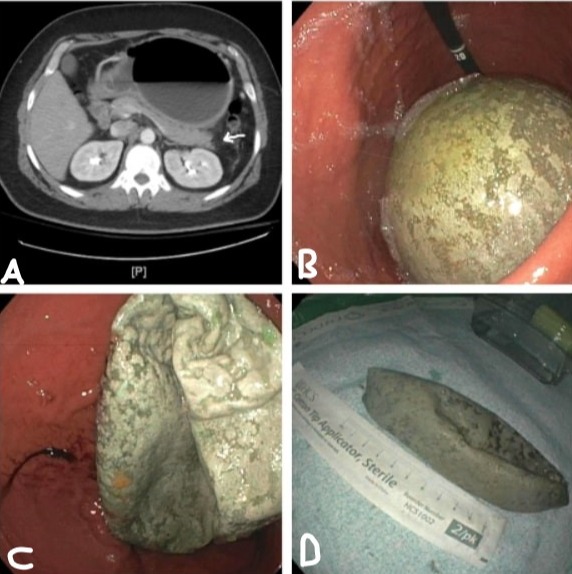
Figure: Figure 1: A. Axial CT scan view shows gastric overdistention with fat standing and fluid collection around the tail of the pancreas. B/C/D shows intragastric balloon decompression and endoscopic removal.
Disclosures:
Mina Alkomos indicated no relevant financial relationships.
Alisa Farokhian indicated no relevant financial relationships.
Nagihan Orhun indicated no relevant financial relationships.
Furqan Bhullar indicated no relevant financial relationships.
Nida Ansari indicated no relevant financial relationships.
Nader Mekheal indicated no relevant financial relationships.
Beshoy Effat Elkomos indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Kamal Amer indicated no relevant financial relationships.
Mina Alkomos, MD1, Alisa Farokhian, MD1, Nagihan Orhun, MD1, Furqan Bhullar, MD1, Nida Ansari, MD1, Nader Mekheal, MD1, Beshoy Effat Elkomos, MD2, Yana Cavanagh, MD1, Walid Baddoura, MD1, Kamal Amer, MD1. P1457 - Intragastric Balloon-Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
