Sunday Poster Session
Category: Obesity
P1459 - Splenic Artery Thrombosis and Glucagon-like Peptide-1 (GLP-1) Agonist: Is There an Association?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Regis Lee, DO
HCA Riverside Community Hospital
Riverside, CA
Presenting Author(s)
Regis Lee, DO1, Joseph J. Alukal, MD2
1HCA Riverside Community Hospital, Riverside, CA; 2University of California Riverside, Riverside, CA
Introduction: Splenic infarcts result from alterations of the blood supply to the spleen. They can be venous or arterial in nature but are usually the result of a clear underlying etiology. We report a case of splenic artery thrombosis which may be associated with use of the glucagon-like peptide (GLP-1) agonist, Semaglutide.
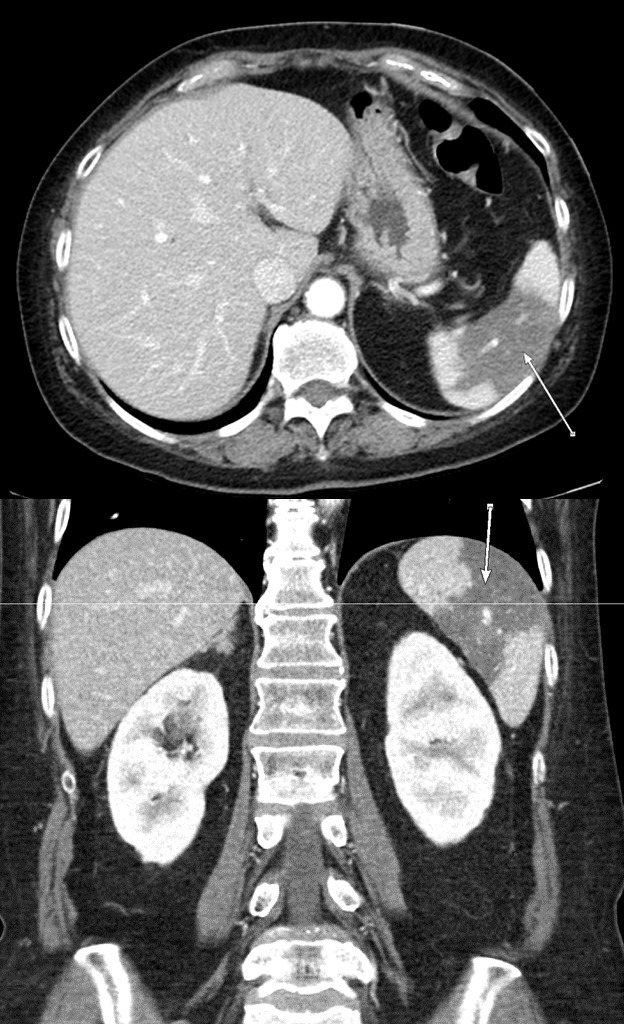
Case Description/Methods: A 59-year-old female with a history of diabetes and obesity (BMI 30) presented to the ED with left upper quadrant abdominal pain, nausea and non-bloody emesis for 2 days. The pain was described as dull, aching, non-radiating, and unrelated to food intake. She denied any associated fever, diarrhea, constipation, or trauma. Surgical history was pertinent for partial sigmoid colon resection over 10 years ago. On admission, her vital signs and laboratory panel were unrevealing, except for an A1C of 7.5. Examination demonstrated significant tenderness to palpation of the left hypochondriac and epigastric regions. Home medications included Glipizide, Metformin, and Pioglitazone. She started on Semaglutide (1 mg weekly) approximately 12 months ago and reported a 40 lb weight loss on it along with improvement in her A1C. CT abdomen with intravenous contrast showed a 7.5 x 4.2 cm hypoenhancement of the mid aspect of the spleen suspicious for splenic infarction, and no evidence of liver disease. CT angiography of the abdomen with intravenous contrast confirmed a filling defect in the distal splenic artery compatible with thrombosis. Hypercoagulability workup revealed normal levels of PT, INR, PTT, factor VIII, homocysteine, and fibrinogen. There was no evidence of atrial fibrillation and echocardiogram showed no cardioembolic source. She was started on therapeutic anticoagulation with heparin and narcotics for pain control. Her abdominal pain improved after approximately 3 days and was discharged home on Apixaban.
Discussion: Splenic infarcts can have atypical presentations affecting patients of all ages. The two most common etiologies are from a thromboembolic or hematological origin. Studies have shown increased GLP-1 levels leading to colonic ischemia (1). Decrease in motility and vascular blood flow can promote thrombosis. This case represents a patient with no known underlying etiology developing splenic infarct in the presence of a GLP-1 agonist. Due to the novelty and increased popularity of Semaglutide, further investigation needs to be performed on possible adverse effects.
1) Wichelmann et al., The American Journal of Gastroenterology, Oct 2022, 117(10S):p e1424
Disclosures:
Regis Lee, DO1, Joseph J. Alukal, MD2. P1459 - Splenic Artery Thrombosis and Glucagon-like Peptide-1 (GLP-1) Agonist: Is There an Association?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Riverside Community Hospital, Riverside, CA; 2University of California Riverside, Riverside, CA
Introduction: Splenic infarcts result from alterations of the blood supply to the spleen. They can be venous or arterial in nature but are usually the result of a clear underlying etiology. We report a case of splenic artery thrombosis which may be associated with use of the glucagon-like peptide (GLP-1) agonist, Semaglutide.
Case Description/Methods: A 59-year-old female with a history of diabetes and obesity (BMI 30) presented to the ED with left upper quadrant abdominal pain, nausea and non-bloody emesis for 2 days. The pain was described as dull, aching, non-radiating, and unrelated to food intake. She denied any associated fever, diarrhea, constipation, or trauma. Surgical history was pertinent for partial sigmoid colon resection over 10 years ago. On admission, her vital signs and laboratory panel were unrevealing, except for an A1C of 7.5. Examination demonstrated significant tenderness to palpation of the left hypochondriac and epigastric regions. Home medications included Glipizide, Metformin, and Pioglitazone. She started on Semaglutide (1 mg weekly) approximately 12 months ago and reported a 40 lb weight loss on it along with improvement in her A1C. CT abdomen with intravenous contrast showed a 7.5 x 4.2 cm hypoenhancement of the mid aspect of the spleen suspicious for splenic infarction, and no evidence of liver disease. CT angiography of the abdomen with intravenous contrast confirmed a filling defect in the distal splenic artery compatible with thrombosis. Hypercoagulability workup revealed normal levels of PT, INR, PTT, factor VIII, homocysteine, and fibrinogen. There was no evidence of atrial fibrillation and echocardiogram showed no cardioembolic source. She was started on therapeutic anticoagulation with heparin and narcotics for pain control. Her abdominal pain improved after approximately 3 days and was discharged home on Apixaban.
Discussion: Splenic infarcts can have atypical presentations affecting patients of all ages. The two most common etiologies are from a thromboembolic or hematological origin. Studies have shown increased GLP-1 levels leading to colonic ischemia (1). Decrease in motility and vascular blood flow can promote thrombosis. This case represents a patient with no known underlying etiology developing splenic infarct in the presence of a GLP-1 agonist. Due to the novelty and increased popularity of Semaglutide, further investigation needs to be performed on possible adverse effects.
1) Wichelmann et al., The American Journal of Gastroenterology, Oct 2022, 117(10S):p e1424
Figure: Arrow indicating splenic infarct.
Disclosures:
Regis Lee indicated no relevant financial relationships.
Joseph Alukal indicated no relevant financial relationships.
Regis Lee, DO1, Joseph J. Alukal, MD2. P1459 - Splenic Artery Thrombosis and Glucagon-like Peptide-1 (GLP-1) Agonist: Is There an Association?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
