Sunday Poster Session
Category: Pediatrics
P1460 - EUS-Guided Drainage With LAMS in Pediatric Perirectal Abscesses: Indications, Outcomes, and Safety
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Aarushi Sudan, MD
NYC Health + Hospitals/Jacobi
New York, NY
Presenting Author(s)
Aarushi Sudan, MD1, Elias Estifan, MD2, Darshana Prem Anand, MD1, Ahan Bhatt, MD3, Sammy Ho, MD2, Inna Novak, MD4
1NYC Health + Hospitals/Jacobi, New York, NY; 2Montefiore Medical Center, New York, NY; 3Albert Einstein College of Medicine, New York, NY; 4Hackensack University Medical Center, Hackensack, NJ
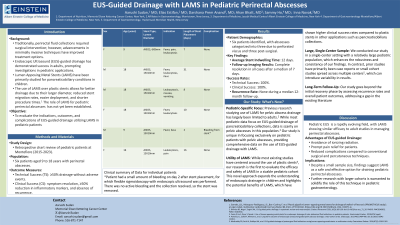
Introduction: Previously necessitating surgical intervention, fluid collections around the rectum can now be effectively drained through minimally invasive methods. The success of Endoscopic Ultrasound (EUS)-guided drainage for abdominal fluid collections in adults has prompted exploration of its application in the pediatric population. EUS guided drainage with Lumen Apposing Metal Stent (LAMS) placement has mainly been studied for pancreaticobiliary etiologies in children. However, the utilization of LAMS for pediatric perirectal abscesses remains an area where its role is yet to be established. In this study, we aim to assess the indications, outcomes, and complications associated with EUS-guided drainage utilizing LAMS placement in pediatric patients at our institution.
Methods: A retrospective chart review was conducted on pediatric patients who underwent EUS-guided drainage of perirectal fluid collections using LAMS at Montefiore between 2015 and 2023. We identified six patients aged 9 to 18 years. The main outcome measures included technical and clinical success and associated adverse events with LAMS placement. Technical success (TS) was defined as ≥50% drainage of the fluid collection without adverse events, while clinical success (CS) encompassed symptom resolution, ≥50% reduction in inflammatory parameters, and absence of recurrences.
Results: Six patients with perirectal abscesses were identified. Among these, three abscesses resulted from a perforated viscus, while three were post-surgical. The average indwelling time for the perirectal abscess stent was 12 days. Follow-up imaging performed after a median of 7 days revealed complete resolution of abscesses in all patients. Stents were then endoscopically removed using a snare. Technical and clinical success rates were both 100%. No recurrences were observed during a median 12-month follow-up.
Discussion: Pediatric EUS is a rapidly evolving field, paralleling its advancements in adult patients. Similar to adults, the application of LAMS can achieve outstanding results in treating perirectal abscesses in the pediatric population. EUS-guided drainage offers significant advantages, including the avoidance of ionizing radiation, prompt pain relief, and a reduction in adverse events compared to conventional surgical and percutaneous alternatives. Despite the limitation in the number of patients included in our study, our findings underscore the efficacy and safety of utilizing LAMS for draining perirectal abscesses in pediatric patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aarushi Sudan, MD1, Elias Estifan, MD2, Darshana Prem Anand, MD1, Ahan Bhatt, MD3, Sammy Ho, MD2, Inna Novak, MD4. P1460 - EUS-Guided Drainage With LAMS in Pediatric Perirectal Abscesses: Indications, Outcomes, and Safety, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYC Health + Hospitals/Jacobi, New York, NY; 2Montefiore Medical Center, New York, NY; 3Albert Einstein College of Medicine, New York, NY; 4Hackensack University Medical Center, Hackensack, NJ
Introduction: Previously necessitating surgical intervention, fluid collections around the rectum can now be effectively drained through minimally invasive methods. The success of Endoscopic Ultrasound (EUS)-guided drainage for abdominal fluid collections in adults has prompted exploration of its application in the pediatric population. EUS guided drainage with Lumen Apposing Metal Stent (LAMS) placement has mainly been studied for pancreaticobiliary etiologies in children. However, the utilization of LAMS for pediatric perirectal abscesses remains an area where its role is yet to be established. In this study, we aim to assess the indications, outcomes, and complications associated with EUS-guided drainage utilizing LAMS placement in pediatric patients at our institution.
Methods: A retrospective chart review was conducted on pediatric patients who underwent EUS-guided drainage of perirectal fluid collections using LAMS at Montefiore between 2015 and 2023. We identified six patients aged 9 to 18 years. The main outcome measures included technical and clinical success and associated adverse events with LAMS placement. Technical success (TS) was defined as ≥50% drainage of the fluid collection without adverse events, while clinical success (CS) encompassed symptom resolution, ≥50% reduction in inflammatory parameters, and absence of recurrences.
Results: Six patients with perirectal abscesses were identified. Among these, three abscesses resulted from a perforated viscus, while three were post-surgical. The average indwelling time for the perirectal abscess stent was 12 days. Follow-up imaging performed after a median of 7 days revealed complete resolution of abscesses in all patients. Stents were then endoscopically removed using a snare. Technical and clinical success rates were both 100%. No recurrences were observed during a median 12-month follow-up.
Discussion: Pediatric EUS is a rapidly evolving field, paralleling its advancements in adult patients. Similar to adults, the application of LAMS can achieve outstanding results in treating perirectal abscesses in the pediatric population. EUS-guided drainage offers significant advantages, including the avoidance of ionizing radiation, prompt pain relief, and a reduction in adverse events compared to conventional surgical and percutaneous alternatives. Despite the limitation in the number of patients included in our study, our findings underscore the efficacy and safety of utilizing LAMS for draining perirectal abscesses in pediatric patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aarushi Sudan indicated no relevant financial relationships.
Elias Estifan indicated no relevant financial relationships.
Darshana Prem Anand indicated no relevant financial relationships.
Ahan Bhatt indicated no relevant financial relationships.
Sammy Ho indicated no relevant financial relationships.
Inna Novak indicated no relevant financial relationships.
Aarushi Sudan, MD1, Elias Estifan, MD2, Darshana Prem Anand, MD1, Ahan Bhatt, MD3, Sammy Ho, MD2, Inna Novak, MD4. P1460 - EUS-Guided Drainage With LAMS in Pediatric Perirectal Abscesses: Indications, Outcomes, and Safety, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
