Sunday Poster Session
Category: Pediatrics
P1461 - Which Serum Biomarker to Choose? Comparing Diagnostic Performance of ESR, CRP, NLR, & PLR for Pediatric Crohn’s Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Akif Shameem, MD
The Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Akif Shameem, MD, Noah Kondamudi, MD
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: According to the American Academy of Pediatrics, up to 5% of pediatric primary care visits are for abdominal pain. With the rising prevalence of pediatric Crohn’s Disease (CD), an estimated 45.9 per 100,000 children, CD should be increasingly considered in the differential diagnoses. Unfortunately, previous studies have demonstrated the diagnostic delay of CD to be 5 months (IQR 4-7.2m). Delayed diagnosis can increase children’s susceptibility to extraintestinal manifestations of IBD including growth and pubertal delay. Adult studies have demonstrated Neutrophil-to-Lymphocyte Ratio (NLR) and Platelet-to-Lymphocyte Ratio (PLR) as alternative markers of inflammation; however, the diagnostic ability of NLR and PLR has not been investigated in pediatric Crohn’s Disease.
Objective:
Primary: To evaluate the diagnostic performance of NLR and PLR for pediatric Crohn’s Disease
Secondary: To compare NLR and PLR to ESR and CRP as diagnostic biomarkers
Methods: A retrospective chart review was performed of patients under 21 years of age, between 2018 and 2022, with endoscopically confirmed CD seen in our outpatient Pediatric GI Clinic. Using the Pediatric Crohn’s Disease Activity Index (PCDAI), each encounter was stratified as inactive (Score < 10) and active (Score ≥ 10). Statistical comparisons, including Independent T-Test, Spearman’s Correlation, and ROC analysis were performed with NLR, PLR, ESR, and CRP.
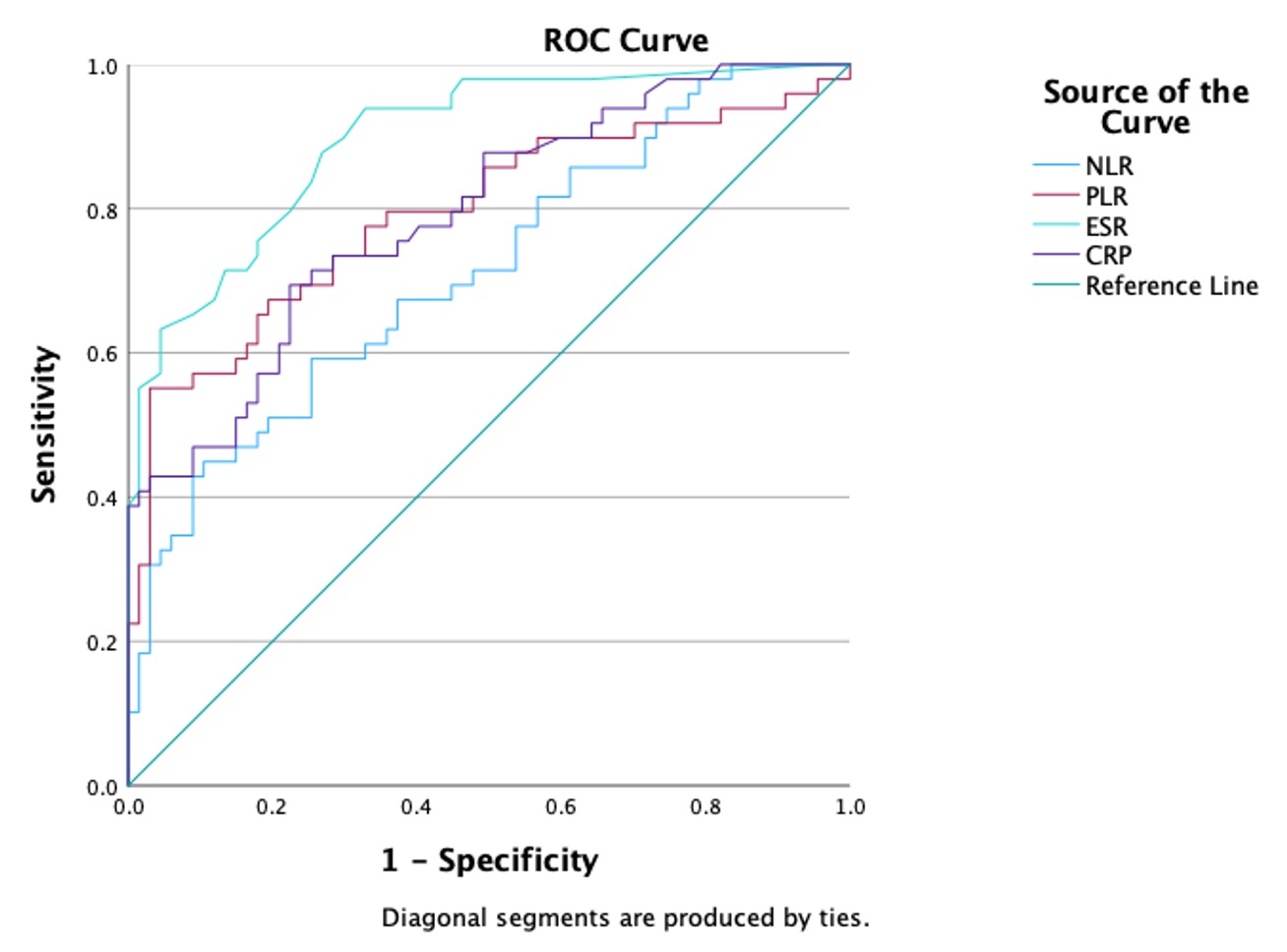
Results: Our study included a total of 134 Crohn’s Disease patient encounters, with 80 inactive and 54 active disease processes. As demonstrated in the table, NLR, PLR, ESR, and CRP were all statistically elevated with a positive correlation with pediatric Crohn’s Disease activity. A ROC analysis demonstrates the AUC for NLR (0.714), PLR (0.776), ESR (0.896), and CRP (0.792). For NLR, a cutoff of 2.07 gives a sensitivity of 0.714 and a specificity of 0.522. For PLR, a cutoff of 182.34 indicates a sensitivity of 0.776 and a specificity of 0.672.
Discussion: Our results demonstrate NLR and PLR have similar diagnostic performance to ESR and CRP for pediatric Crohn’s Disease. However, the major advantage of NLR and PLR is that these ratios can be calculated from a routine CBC, which is more readily available and more inexpensive compared to traditional inflammatory blood tests. The similar efficacy with reduced costs, makes NLR and PLR ideal alternative diagnostic markers for pediatric Crohn’s Disease.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Akif Shameem, MD, Noah Kondamudi, MD. P1461 - Which Serum Biomarker to Choose? Comparing Diagnostic Performance of ESR, CRP, NLR, & PLR for Pediatric Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: According to the American Academy of Pediatrics, up to 5% of pediatric primary care visits are for abdominal pain. With the rising prevalence of pediatric Crohn’s Disease (CD), an estimated 45.9 per 100,000 children, CD should be increasingly considered in the differential diagnoses. Unfortunately, previous studies have demonstrated the diagnostic delay of CD to be 5 months (IQR 4-7.2m). Delayed diagnosis can increase children’s susceptibility to extraintestinal manifestations of IBD including growth and pubertal delay. Adult studies have demonstrated Neutrophil-to-Lymphocyte Ratio (NLR) and Platelet-to-Lymphocyte Ratio (PLR) as alternative markers of inflammation; however, the diagnostic ability of NLR and PLR has not been investigated in pediatric Crohn’s Disease.
Objective:
Primary: To evaluate the diagnostic performance of NLR and PLR for pediatric Crohn’s Disease
Secondary: To compare NLR and PLR to ESR and CRP as diagnostic biomarkers
Methods: A retrospective chart review was performed of patients under 21 years of age, between 2018 and 2022, with endoscopically confirmed CD seen in our outpatient Pediatric GI Clinic. Using the Pediatric Crohn’s Disease Activity Index (PCDAI), each encounter was stratified as inactive (Score < 10) and active (Score ≥ 10). Statistical comparisons, including Independent T-Test, Spearman’s Correlation, and ROC analysis were performed with NLR, PLR, ESR, and CRP.
Results: Our study included a total of 134 Crohn’s Disease patient encounters, with 80 inactive and 54 active disease processes. As demonstrated in the table, NLR, PLR, ESR, and CRP were all statistically elevated with a positive correlation with pediatric Crohn’s Disease activity. A ROC analysis demonstrates the AUC for NLR (0.714), PLR (0.776), ESR (0.896), and CRP (0.792). For NLR, a cutoff of 2.07 gives a sensitivity of 0.714 and a specificity of 0.522. For PLR, a cutoff of 182.34 indicates a sensitivity of 0.776 and a specificity of 0.672.
Discussion: Our results demonstrate NLR and PLR have similar diagnostic performance to ESR and CRP for pediatric Crohn’s Disease. However, the major advantage of NLR and PLR is that these ratios can be calculated from a routine CBC, which is more readily available and more inexpensive compared to traditional inflammatory blood tests. The similar efficacy with reduced costs, makes NLR and PLR ideal alternative diagnostic markers for pediatric Crohn’s Disease.
Figure: ROC for Serum Biomarkers
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Akif Shameem indicated no relevant financial relationships.
Noah Kondamudi indicated no relevant financial relationships.
Akif Shameem, MD, Noah Kondamudi, MD. P1461 - Which Serum Biomarker to Choose? Comparing Diagnostic Performance of ESR, CRP, NLR, & PLR for Pediatric Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
