Sunday Poster Session
Category: Pediatrics
P1484 - Choledochocele in a Pediatric Patient With Pancreaticobiliary Maljunction
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hannah L. Bell, BS
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Monica Moreno, 1, Hannah Bell, 1, Faisal A.. Bukeirat, MD2, Abdallah Abdallah, MD1
1University of Mississippi Medical Center, Jackson, MS; 2UMMC, Jackson, MS
Introduction: Pancreaticobiliary maljunction (PBM) is a congenital anomaly that describes the connection of the bile and pancreatic ducts outside of the duodenum, and predisposes patients to malignancies of the gallbladder and biliary tract. There are two types of PBM: PBM with and without biliary dilation. Choledochal cysts (CC) arise due to dilation of this malformed duct, and are often diagnosed in the early stages of life in one out of every 100,000-150,000 children in Western countries.
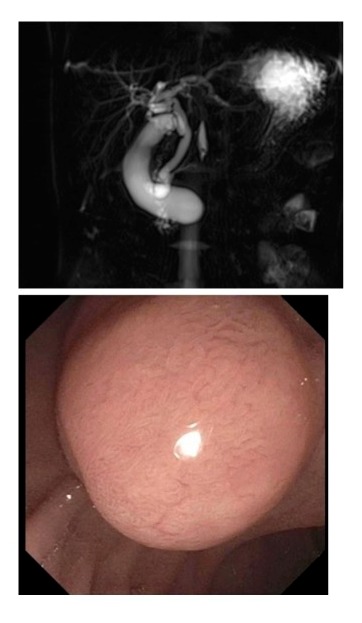
Case Description/Methods: A 10-year-old male presented to an outside hospital with three-days of non-bilious, non-bloody emesis, right upper quadrant pain, nausea, and fever. Prior to presentation, intermittent abdominal pain for a few months before it worsened and became persistent. Initial laboratory tests revealed elevated liver enzymes (AST 268 U/L, ALT 361 U/L), alkaline phosphatase (689 U/L), total bilirubin (6.7 mg/dL), direct bilirubin (5.6 mg/dL), and lipase (1491 U/L). A computed tomography (CT) scan showed a dilated common bile duct (CBD) measuring 10 mm with a cystic structure, raising concerns for a CC. Upon transfer, liver enzymes were persistently elevated (ALT 350 U/L, AST 261 U/L), alkaline phosphatase (580 U/L), total bilirubin (2.4 mg/dL), and direct bilirubin (1.78 mg/dL). A gallbladder ultrasound revealed dependent sludge, but no stones. Magnetic resonance cholangiopancreatography (MRCP) confirmed CC with cystic dilatation measuring about 1.2cm at the confluence of the common and pancreatic ducts, along with an anomalous pancreaticobiliary junction. Endoscopic retrograde cholangiopancreatography (ERCP) identified a choledochocele causing an obstruction. The main bile duct was mildly and diffusely dilated with the largest ductal diameter measuring 6mm. A therapeutic biliary sphincterotomy with dissection through the cyst was performed and the lining of the choledochocele was biopsied, showing both duodenal and biliary epithelium without dysplasia.
Discussion: PBM and resulting CC formation predispose patients to pancreatitis and cholangiocarcinoma. Both classifications of PBM are at increased risk for gallbladder and biliary tract malignancies. Recognizing and treating PBM through appropriate procedures and surgeries is critical to avoiding progression of cancer, especially in those without ductal dilatation who are asymptomatic for longer periods of time, resulting in more advanced malignancies.
Disclosures:
Monica Moreno, 1, Hannah Bell, 1, Faisal A.. Bukeirat, MD2, Abdallah Abdallah, MD1. P1484 - Choledochocele in a Pediatric Patient With Pancreaticobiliary Maljunction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Mississippi Medical Center, Jackson, MS; 2UMMC, Jackson, MS
Introduction: Pancreaticobiliary maljunction (PBM) is a congenital anomaly that describes the connection of the bile and pancreatic ducts outside of the duodenum, and predisposes patients to malignancies of the gallbladder and biliary tract. There are two types of PBM: PBM with and without biliary dilation. Choledochal cysts (CC) arise due to dilation of this malformed duct, and are often diagnosed in the early stages of life in one out of every 100,000-150,000 children in Western countries.
Case Description/Methods: A 10-year-old male presented to an outside hospital with three-days of non-bilious, non-bloody emesis, right upper quadrant pain, nausea, and fever. Prior to presentation, intermittent abdominal pain for a few months before it worsened and became persistent. Initial laboratory tests revealed elevated liver enzymes (AST 268 U/L, ALT 361 U/L), alkaline phosphatase (689 U/L), total bilirubin (6.7 mg/dL), direct bilirubin (5.6 mg/dL), and lipase (1491 U/L). A computed tomography (CT) scan showed a dilated common bile duct (CBD) measuring 10 mm with a cystic structure, raising concerns for a CC. Upon transfer, liver enzymes were persistently elevated (ALT 350 U/L, AST 261 U/L), alkaline phosphatase (580 U/L), total bilirubin (2.4 mg/dL), and direct bilirubin (1.78 mg/dL). A gallbladder ultrasound revealed dependent sludge, but no stones. Magnetic resonance cholangiopancreatography (MRCP) confirmed CC with cystic dilatation measuring about 1.2cm at the confluence of the common and pancreatic ducts, along with an anomalous pancreaticobiliary junction. Endoscopic retrograde cholangiopancreatography (ERCP) identified a choledochocele causing an obstruction. The main bile duct was mildly and diffusely dilated with the largest ductal diameter measuring 6mm. A therapeutic biliary sphincterotomy with dissection through the cyst was performed and the lining of the choledochocele was biopsied, showing both duodenal and biliary epithelium without dysplasia.
Discussion: PBM and resulting CC formation predispose patients to pancreatitis and cholangiocarcinoma. Both classifications of PBM are at increased risk for gallbladder and biliary tract malignancies. Recognizing and treating PBM through appropriate procedures and surgeries is critical to avoiding progression of cancer, especially in those without ductal dilatation who are asymptomatic for longer periods of time, resulting in more advanced malignancies.
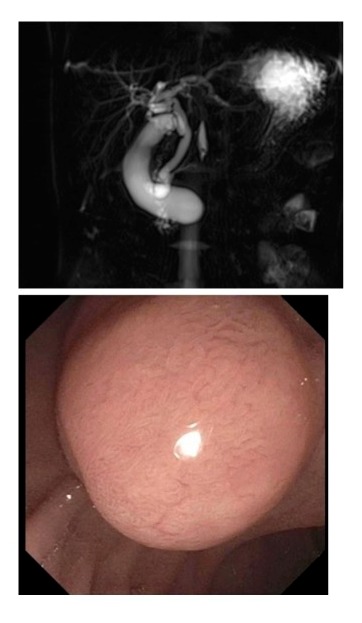
Figure: Image 1: MRCP CC with cystic dilatation measuring about 1.2cm at the confluence of the common and pancreatic ducts, along with an anomalous pancreaticobiliary junction.
Image 2: Choledochal Cyst
Image 2: Choledochal Cyst
Disclosures:
Monica Moreno indicated no relevant financial relationships.
Hannah Bell indicated no relevant financial relationships.
Faisal Bukeirat indicated no relevant financial relationships.
Abdallah Abdallah indicated no relevant financial relationships.
Monica Moreno, 1, Hannah Bell, 1, Faisal A.. Bukeirat, MD2, Abdallah Abdallah, MD1. P1484 - Choledochocele in a Pediatric Patient With Pancreaticobiliary Maljunction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
