Sunday Poster Session
Category: Practice Management
P1507 - A Standardized, Specialty-Specific Note Template Improves Inpatient Evaluation and Management Coding Capture
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Joshua L. Hudson, MD, MSc
University of North Carolina at Chapel Hill School of Medicine
Chapel Hill, NC
Presenting Author(s)
Award: ACG Outstanding Research Award in the Practice Management Category
Award: Presidential Poster Award
Joshua L. Hudson, MD, MSc1, Rachel Knight, BA2, Shifali Arora, MD1
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2University of North Carolina Hospitals, Chapel Hill, NC
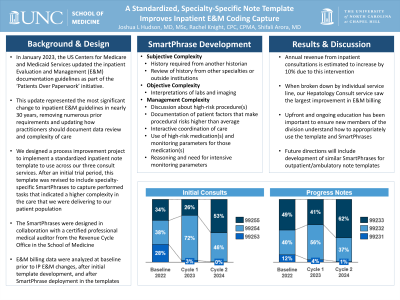
Introduction: The required components for documentation changed in January 2021 as part of the government’s ‘Patients over Paperwork’ initiative. These were the most significant updates to the evaluation and management (E/M) guidelines in 25 years. We sought to design a process improvement project to standardize the note template used by our inpatient consult teams to adhere to these new guidelines and capture the complexity of E/M services provided to our patients.
Methods: An initial cycle of change was implemented in January 2023, during which a standardized note template was published that adhered to the 2021 E/M changes. Baseline E/M coding was then compared to E/M coding after this initial cycle of change. The note template was then reviewed with a certified professional medical auditor from the revenue cycle department to identify areas where the template was deficient in capturing complexity of care. A second cycle of change was implemented in January 2024 introducing SmartPhrases to capture data review and specialty-specific items that captured complexity of care. After this cycle, E/M coding was again compared to baseline coding and coding after the first cycle of change. All clinicians were educated about the changes with each cycle of change.
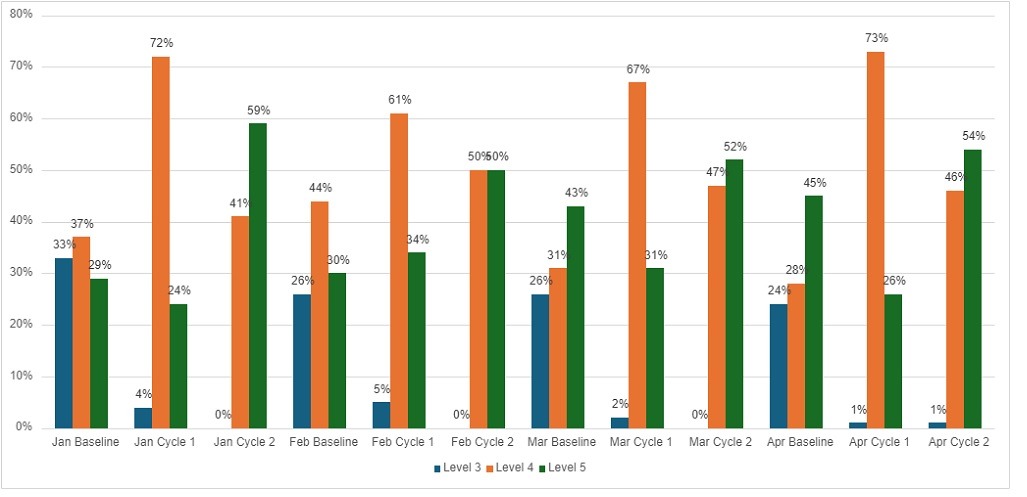
Results: Baseline data revealed that new inpatient consultations were on average coded 27% as 99253 (low), 35% as 99254 (mid), and 37% as 99255 (high). After both rounds of changes, new inpatient consultations were on average coded 0% as 99253, 46% as 99254, and 54% as 99255. Baseline data for follow-up hospital care were on average coded 12% as 99231 (low), 41% as 99232 (mid), and 48% as 99233 (high). After both rounds of changes, follow-up hospital care visits were on average coded 1% as 99231, 38% as 99232, and 61% as 99233. These changes to documentation are estimated to increase inpatient consultation revenue by approximately 10% annually without any substantial change in workflow for clinicians.
Discussion: Our project demonstrates that standardization of documentation along with development of specialty-specific SmartPhrases can improve physician E/M coding. Partnering with an auditor with coding experience and development of 3 SmartPhrases was key to the success of this project. The SmartPhrases were designed to capture important elements of record review, data review, and factors that influence complexity of care delivered including risks associated with procedures, patient factors that increased procedural risk, and coordination of care.
Disclosures:
Joshua L. Hudson, MD, MSc1, Rachel Knight, BA2, Shifali Arora, MD1. P1507 - A Standardized, Specialty-Specific Note Template Improves Inpatient Evaluation and Management Coding Capture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Award: Presidential Poster Award
Joshua L. Hudson, MD, MSc1, Rachel Knight, BA2, Shifali Arora, MD1
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2University of North Carolina Hospitals, Chapel Hill, NC
Introduction: The required components for documentation changed in January 2021 as part of the government’s ‘Patients over Paperwork’ initiative. These were the most significant updates to the evaluation and management (E/M) guidelines in 25 years. We sought to design a process improvement project to standardize the note template used by our inpatient consult teams to adhere to these new guidelines and capture the complexity of E/M services provided to our patients.
Methods: An initial cycle of change was implemented in January 2023, during which a standardized note template was published that adhered to the 2021 E/M changes. Baseline E/M coding was then compared to E/M coding after this initial cycle of change. The note template was then reviewed with a certified professional medical auditor from the revenue cycle department to identify areas where the template was deficient in capturing complexity of care. A second cycle of change was implemented in January 2024 introducing SmartPhrases to capture data review and specialty-specific items that captured complexity of care. After this cycle, E/M coding was again compared to baseline coding and coding after the first cycle of change. All clinicians were educated about the changes with each cycle of change.
Results: Baseline data revealed that new inpatient consultations were on average coded 27% as 99253 (low), 35% as 99254 (mid), and 37% as 99255 (high). After both rounds of changes, new inpatient consultations were on average coded 0% as 99253, 46% as 99254, and 54% as 99255. Baseline data for follow-up hospital care were on average coded 12% as 99231 (low), 41% as 99232 (mid), and 48% as 99233 (high). After both rounds of changes, follow-up hospital care visits were on average coded 1% as 99231, 38% as 99232, and 61% as 99233. These changes to documentation are estimated to increase inpatient consultation revenue by approximately 10% annually without any substantial change in workflow for clinicians.
Discussion: Our project demonstrates that standardization of documentation along with development of specialty-specific SmartPhrases can improve physician E/M coding. Partnering with an auditor with coding experience and development of 3 SmartPhrases was key to the success of this project. The SmartPhrases were designed to capture important elements of record review, data review, and factors that influence complexity of care delivered including risks associated with procedures, patient factors that increased procedural risk, and coordination of care.
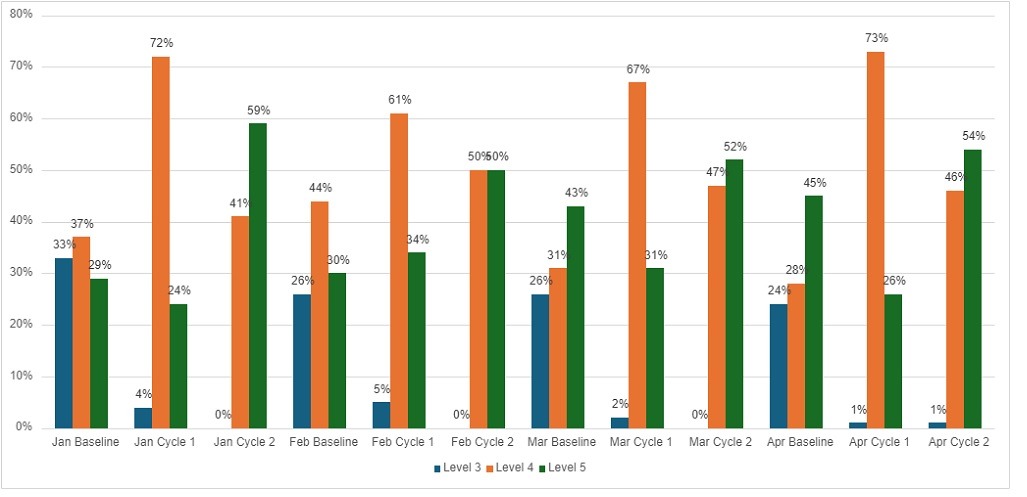
Figure: Month-over-Month Change in Billing Codes for Initial Consults
Jan=January, Feb=February, Mar=March, Apr=April
Jan=January, Feb=February, Mar=March, Apr=April
Disclosures:
Joshua Hudson indicated no relevant financial relationships.
Rachel Knight indicated no relevant financial relationships.
Shifali Arora indicated no relevant financial relationships.
Joshua L. Hudson, MD, MSc1, Rachel Knight, BA2, Shifali Arora, MD1. P1507 - A Standardized, Specialty-Specific Note Template Improves Inpatient Evaluation and Management Coding Capture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


