Sunday Poster Session
Category: Small Intestine
P1558 - Coexistence of Intestinal Spirochetosis and Colorectal Cancer: Could the Coil Be Carcinogenic?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Hannah L. Zuercher, MD
University of Florida College of Medicine
Gainesville, FL
Presenting Author(s)
Hannah L. Zuercher, MD1, Arvin Daneshmand, MD1, Eugene Stolow, MD1, Matthew Giansiracusa, DO1, Antonios Sapounas, MD2
1University of Florida College of Medicine, Gainesville, FL; 2Malcom Randall Veterans Affairs Medical Center, Gainesville, FL
Introduction: Intestinal spirochetosis (IS) is caused by the enteric pathogens Brachyspira aalborgior and Brachyspira pilosicoli. The mechanism for IS pathogenicity consists of defacement of the brush border microvilli. Notably, men who have sex with men and those with human immunodeficiency virus (HIV) have higher prevalence rates. IS often presents clinically with progressive abdominal pain, watery diarrhea and unintentional weight loss. The severity of symptoms fluctuates from asymptomatic to life-threatening manifestations. Present literature does not clearly define the relationship between IS and colorectal malignancy. However, evidence suggests that IS may correlate with enhanced colonic polyp development; hence, the importance of promptly identifying and treating IS.
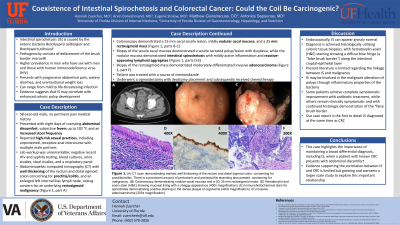
Case Description/Methods: A 58-year-old male with no pertinent past medical history presented with eight days of cramping abdominal discomfort, subjective fevers up to 102 °F, and an increased stool frequency. He reported high-risk sexual practices, including unprotected, receptive anal intercourse with multiple male partners. Lab workup was unremarkable. Recent HIV and syphilis testing had been negative. Abdominopelvic computed tomography (CT) demonstrated marked wall thickening of the rectum and distal sigmoid colon concerning for proctitis/colitis, and an enlarged left internal iliac lymph node raising concern for an underlying rectosigmoid malignancy (Figure 1, part A). Colonoscopy demonstrated a 15 mm cecal sessile lesion, mildly nodular cecal mucosa, and a 35 mm rectosigmoid mass (Figure 1, parts B-C). Biopsy of the sessile cecal mucosa demonstrated a sessile serrated polyp/lesion with dysplasia, while the nodular mucosa demonstrated intestinal spirochetosis with mildly active inflammation and reactive-appearing lymphoid aggregates (Figure 1, parts D-E). Biopsy of the rectosigmoid mass demonstrated moderately-differentiated invasive adenocarcinoma (Figure 1, part F). The patient was treated with a course of metronidazole and underwent a sigmoidectomy with ileostomy placement.
Discussion: This case highlights the importance of maintaining a broad differential diagnosis, including IS when an immunocompromised patient presents with abdominal discomfort. IS is formally diagnosed with endoscopic biopsy, and treatment with antibiotics can result in rapid improvement of symptoms. Evidence supporting the correlation between IS and CRC is limited but growing and warrants a larger scale study to explore this important relationship.

Disclosures:
Hannah L. Zuercher, MD1, Arvin Daneshmand, MD1, Eugene Stolow, MD1, Matthew Giansiracusa, DO1, Antonios Sapounas, MD2. P1558 - Coexistence of Intestinal Spirochetosis and Colorectal Cancer: Could the Coil Be Carcinogenic?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida College of Medicine, Gainesville, FL; 2Malcom Randall Veterans Affairs Medical Center, Gainesville, FL
Introduction: Intestinal spirochetosis (IS) is caused by the enteric pathogens Brachyspira aalborgior and Brachyspira pilosicoli. The mechanism for IS pathogenicity consists of defacement of the brush border microvilli. Notably, men who have sex with men and those with human immunodeficiency virus (HIV) have higher prevalence rates. IS often presents clinically with progressive abdominal pain, watery diarrhea and unintentional weight loss. The severity of symptoms fluctuates from asymptomatic to life-threatening manifestations. Present literature does not clearly define the relationship between IS and colorectal malignancy. However, evidence suggests that IS may correlate with enhanced colonic polyp development; hence, the importance of promptly identifying and treating IS.
Case Description/Methods: A 58-year-old male with no pertinent past medical history presented with eight days of cramping abdominal discomfort, subjective fevers up to 102 °F, and an increased stool frequency. He reported high-risk sexual practices, including unprotected, receptive anal intercourse with multiple male partners. Lab workup was unremarkable. Recent HIV and syphilis testing had been negative. Abdominopelvic computed tomography (CT) demonstrated marked wall thickening of the rectum and distal sigmoid colon concerning for proctitis/colitis, and an enlarged left internal iliac lymph node raising concern for an underlying rectosigmoid malignancy (Figure 1, part A). Colonoscopy demonstrated a 15 mm cecal sessile lesion, mildly nodular cecal mucosa, and a 35 mm rectosigmoid mass (Figure 1, parts B-C). Biopsy of the sessile cecal mucosa demonstrated a sessile serrated polyp/lesion with dysplasia, while the nodular mucosa demonstrated intestinal spirochetosis with mildly active inflammation and reactive-appearing lymphoid aggregates (Figure 1, parts D-E). Biopsy of the rectosigmoid mass demonstrated moderately-differentiated invasive adenocarcinoma (Figure 1, part F). The patient was treated with a course of metronidazole and underwent a sigmoidectomy with ileostomy placement.
Discussion: This case highlights the importance of maintaining a broad differential diagnosis, including IS when an immunocompromised patient presents with abdominal discomfort. IS is formally diagnosed with endoscopic biopsy, and treatment with antibiotics can result in rapid improvement of symptoms. Evidence supporting the correlation between IS and CRC is limited but growing and warrants a larger scale study to explore this important relationship.

Figure: (A) CT scan demonstrating marked wall thickening of the rectum and distal sigmoid colon, concerning for proctitis/colitis. There is a prominent amount of pericolonic and perirectal fat stranding also present, concerning for malignancy. (B) Colonoscopy demonstrating nodular cecal mucosa and a (C) 35 mm rectosigmoid mass. (D) Hematoxylin and eosin stain (H&E) showing mucosal lining with a shaggy appearance (400x magnification). (E) Immunohistochemical stain for spirochetes demonstrating positive staining in the dense plaque of organisms (400x magnification). (F) Invasive adenocarcinoma (200x magnification).
Disclosures:
Hannah Zuercher indicated no relevant financial relationships.
Arvin Daneshmand indicated no relevant financial relationships.
Eugene Stolow indicated no relevant financial relationships.
Matthew Giansiracusa indicated no relevant financial relationships.
Antonios Sapounas indicated no relevant financial relationships.
Hannah L. Zuercher, MD1, Arvin Daneshmand, MD1, Eugene Stolow, MD1, Matthew Giansiracusa, DO1, Antonios Sapounas, MD2. P1558 - Coexistence of Intestinal Spirochetosis and Colorectal Cancer: Could the Coil Be Carcinogenic?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
