Sunday Poster Session
Category: Small Intestine
P1559 - Spontaneous in Hospital Duodenal Bulb Perforation in a Xylazine User
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Himsikhar Khataniar, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Himsikhar Khataniar, MD, Naveed Chaudhry, MD, Ashni Dharia, MD, Akash Gadani, MD
Allegheny General Hospital, Pittsburgh, PA
Introduction: Xylazine, a synthetic veterinary tranquilizer and alpha-adrenergic receptor agonist, was originally developed as an analogue to clonidine. Recent studies have highlighted its severe side effects, including significant respiratory and central nervous system depression, cardiovascular impact, rhabdomyolysis, and the development of necrotic skin ulcers. As the emergence of xylazine amidst the opioid crisis is relatively recent, our understanding of its comprehensive impact on humans is limited by insufficient data.
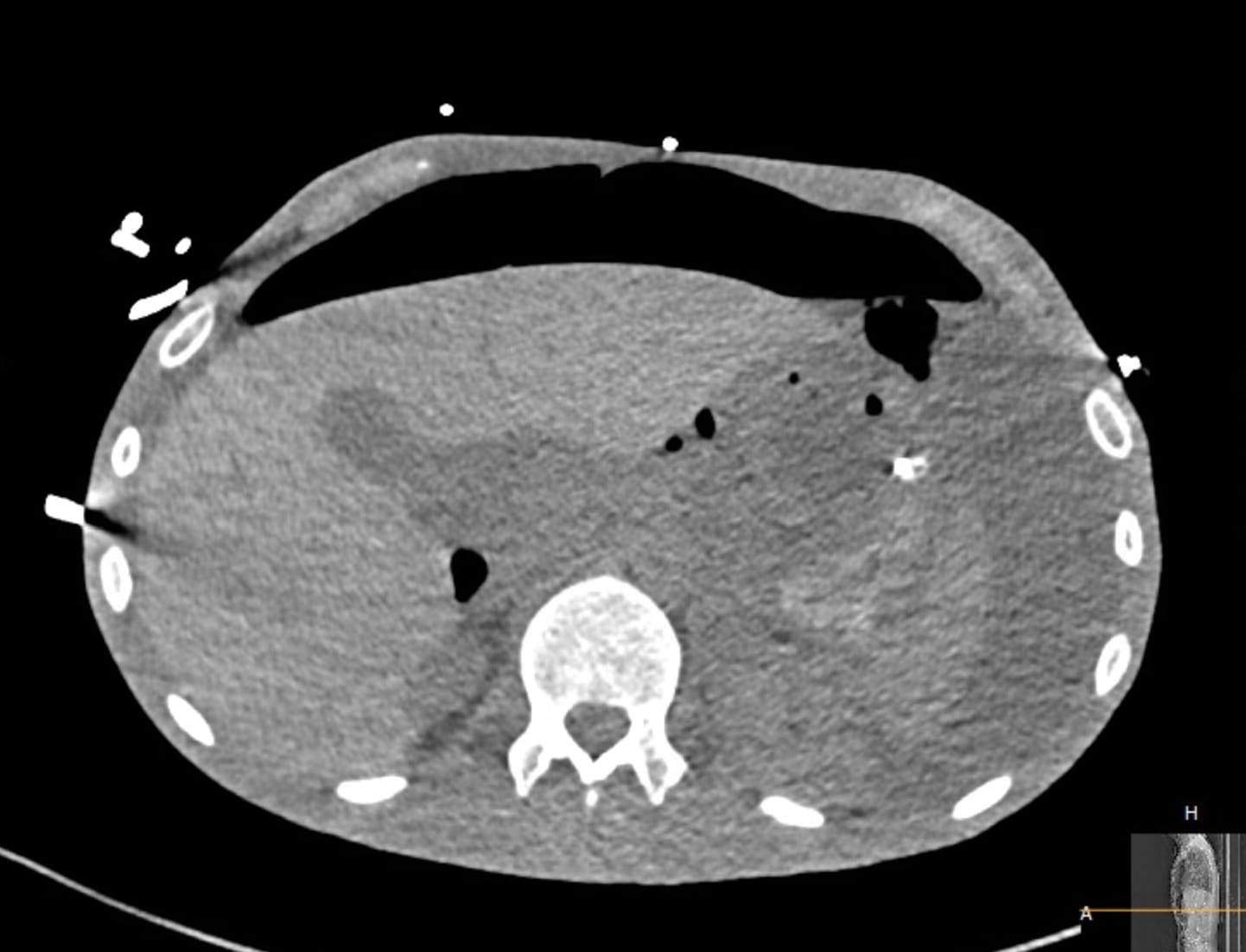
Case Description/Methods: A 41-year-old male presented to the emergency department with symptoms of nausea, vomiting, abdominal pain, and elevated glucose levels. The patient had a history of uncontrolled Type 1 diabetes mellitus, left upper extremity wounds, and polysubstance abuse. On examination, he had a high respiratory rate and lab results consistent with DKA, alongside positive screenings for fentanyl and cocaine (Table 1). The patient's left forearm wound exhibited serous drainage with gram-positive cocci and gram-negative rods. He reported self-injecting xylazine and fentanyl in his arms and hands approximately every four hours over the past year. Despite initial stabilization, the patient remained lethargic. The following night, he experienced severe pain, diaphoresis, and mydriasis, probably associated with opioid withdrawal. His systolic blood pressure dropped to 55 mmHg, and he desaturated despite receiving 15 L of oxygen via nasal cannula. A rapid response team was called, and he was intubated and transferred to the ICU for worsening respiratory failure and altered mental status. A CT angiogram revealed a significant amount of free air and fluid within the peritoneal cavity (Figure 1). An exploratory laparotomy revealed a 1.5 cm full-thickness perforation on the anterior wall of the first portion of the duodenum. A Graham patch repair for the duodenal ulcer and an abdominal cavity washout were performed. The patient’s condition improved over the next five days, and he was discharged home safely.
Discussion: The patient had no prior history of peptic ulcer disease or other significant conditions that could predispose him to duodenal perforation. We deduced that the perforation of his duodenal bulb, likely induced by duodenal ischemia, stemmed from his chronic illicit drug use. This case highlights a potential rare side effect associated with the increasingly prevalent street drug, xylazine.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Himsikhar Khataniar, MD, Naveed Chaudhry, MD, Ashni Dharia, MD, Akash Gadani, MD. P1559 - Spontaneous in Hospital Duodenal Bulb Perforation in a Xylazine User, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Allegheny General Hospital, Pittsburgh, PA
Introduction: Xylazine, a synthetic veterinary tranquilizer and alpha-adrenergic receptor agonist, was originally developed as an analogue to clonidine. Recent studies have highlighted its severe side effects, including significant respiratory and central nervous system depression, cardiovascular impact, rhabdomyolysis, and the development of necrotic skin ulcers. As the emergence of xylazine amidst the opioid crisis is relatively recent, our understanding of its comprehensive impact on humans is limited by insufficient data.
Case Description/Methods: A 41-year-old male presented to the emergency department with symptoms of nausea, vomiting, abdominal pain, and elevated glucose levels. The patient had a history of uncontrolled Type 1 diabetes mellitus, left upper extremity wounds, and polysubstance abuse. On examination, he had a high respiratory rate and lab results consistent with DKA, alongside positive screenings for fentanyl and cocaine (Table 1). The patient's left forearm wound exhibited serous drainage with gram-positive cocci and gram-negative rods. He reported self-injecting xylazine and fentanyl in his arms and hands approximately every four hours over the past year. Despite initial stabilization, the patient remained lethargic. The following night, he experienced severe pain, diaphoresis, and mydriasis, probably associated with opioid withdrawal. His systolic blood pressure dropped to 55 mmHg, and he desaturated despite receiving 15 L of oxygen via nasal cannula. A rapid response team was called, and he was intubated and transferred to the ICU for worsening respiratory failure and altered mental status. A CT angiogram revealed a significant amount of free air and fluid within the peritoneal cavity (Figure 1). An exploratory laparotomy revealed a 1.5 cm full-thickness perforation on the anterior wall of the first portion of the duodenum. A Graham patch repair for the duodenal ulcer and an abdominal cavity washout were performed. The patient’s condition improved over the next five days, and he was discharged home safely.
Discussion: The patient had no prior history of peptic ulcer disease or other significant conditions that could predispose him to duodenal perforation. We deduced that the perforation of his duodenal bulb, likely induced by duodenal ischemia, stemmed from his chronic illicit drug use. This case highlights a potential rare side effect associated with the increasingly prevalent street drug, xylazine.
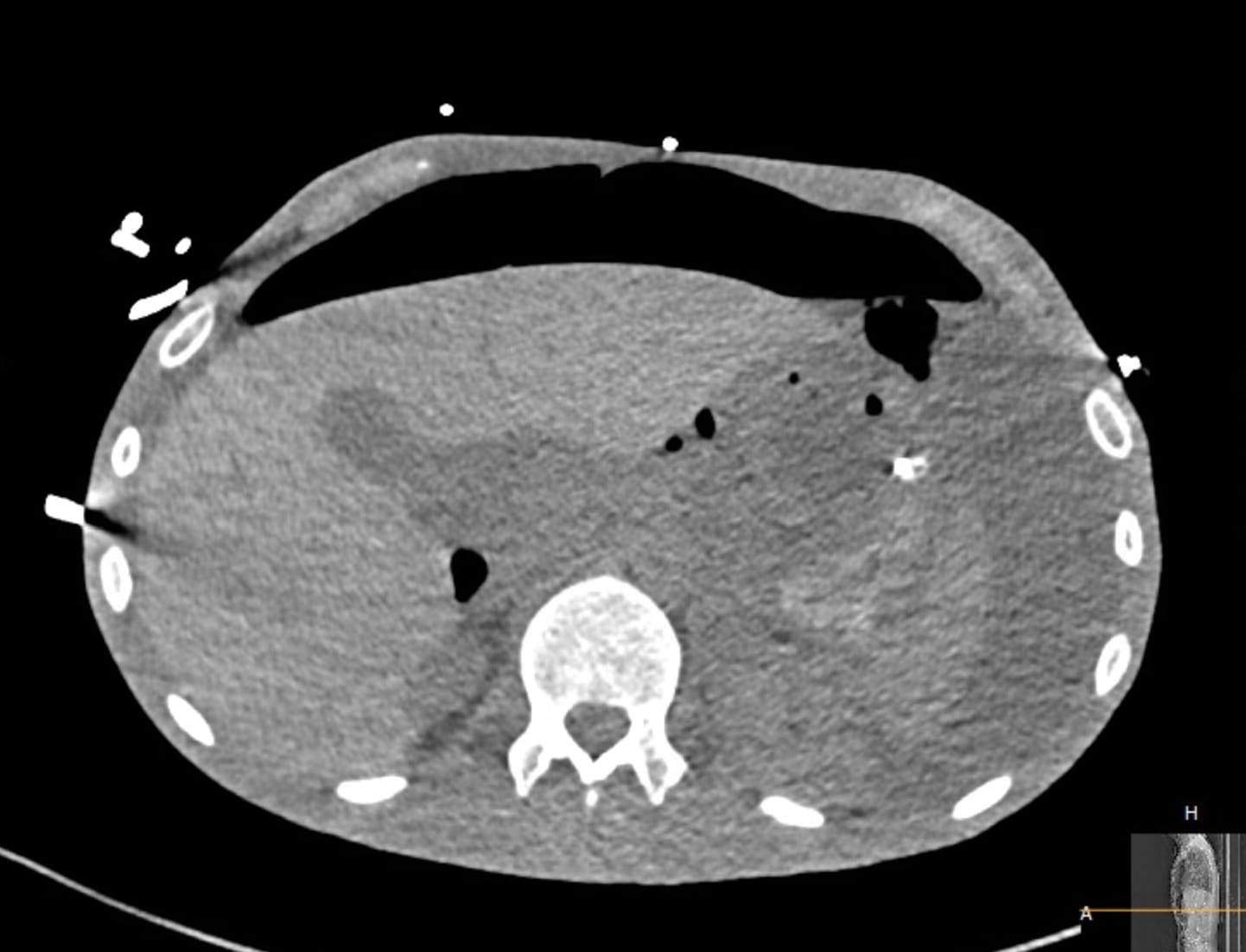
Figure: CT abdomen and pelvis showing pneumoperitoneum and ascites
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Naveed Chaudhry indicated no relevant financial relationships.
Ashni Dharia indicated no relevant financial relationships.
Akash Gadani: Phathom Pharmaceuticals – Speakers Bureau.
Himsikhar Khataniar, MD, Naveed Chaudhry, MD, Ashni Dharia, MD, Akash Gadani, MD. P1559 - Spontaneous in Hospital Duodenal Bulb Perforation in a Xylazine User, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
