Sunday Poster Session
Category: Small Intestine
P1561 - A Case of Small and Large Bowel Ischemic Ulcerations in a Patient With Atypical Hemolytic Uremic Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Mary Camacho, BS
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Mary Camacho, BS1, Julia Massaad, MD1, Lovekirat Dhaliwal, MD1, Lasha Chkhikvadze, 2, Wei Zheng, MD, PhD1
1Emory University School of Medicine, Atlanta, GA; 2Tbilisi State Medical University, Tbilisi, T'bilisi, Georgia
Introduction: Atypical hemolytic uremic syndrome (aHUS) is a rare thrombotic microangiopathy caused by dysregulation of the alternate complement pathway. It is characterized by renal involvement, but extrarenal involvement is common. Gastrointestinal (GI) complications, such as diarrhea, vomiting, GI bleeding, and inflammatory bowel disease (IBD) are common. However, isolated small bowel/colonic ulcerations in aHUS have not been reported. We present a challenging caseof small and large bowel ulcerations in aHUS.
Case Description/Methods: A 36-year-old woman with history of aHUS and secondary end stage renal disease on hemodialysis presented to our emergency department with a 3-month history of severe epigastric pain. She was initially treated with eculizumab loading followed by ravulizumab maintenancetherapy. She had several outside hospitalizations for abdominal pain, diarrhea and vomiting since her diagnosis. Workup included a non-contrast CT scan with terminal ileum (TI), cecal, and ascending colonic thickening. EGD and colonoscopy revealed small duodenal and TI ulcerations, but pathology showed nonspecific inflammation. She was treated with a short course of prednisone and budesonide with possibly mild improvement. On presentation to our center, she had epigastric pain and stable anemia without evidence of hemolysis. Enteroscopy and colonoscopy revealed deep large ulcers in the third and fourth portion of the duodenum, proximaljejunum, and one small superficial ulcer in the cecum. MRI showed mild thickening and hyperemia of jejunal loops. She was initially treated with IV steroids but had no clinical response this time. After review by multiple expert pathologists, it was determined that her ulcerationswere due to microvascular thrombi. Extensive hematologic, autoimmune and infectious workupsfor alternate etiologies were negative. Hematology restarted her on weekly eculizumab loading with significant improvement in her abdominal pain, and she was discharged with close hematology follow up.
Discussion: Intestinal ulcerations in aHUS can develop secondary to microvascular thrombosis and resultantischemia. IBD was considered, but the absence of chronic inflammatory changes on biopsy and lack of response to steroids argue against it. MRI and endoscopic evaluation are crucial for determining the etiology of small bowel ulcerations in aHUS patients. Treatment is primarily aimed at treating the underlying aHUS. To our knowledge, this is a very rare complication with no other cases found in the literature.

Disclosures:
Mary Camacho, BS1, Julia Massaad, MD1, Lovekirat Dhaliwal, MD1, Lasha Chkhikvadze, 2, Wei Zheng, MD, PhD1. P1561 - A Case of Small and Large Bowel Ischemic Ulcerations in a Patient With Atypical Hemolytic Uremic Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Emory University School of Medicine, Atlanta, GA; 2Tbilisi State Medical University, Tbilisi, T'bilisi, Georgia
Introduction: Atypical hemolytic uremic syndrome (aHUS) is a rare thrombotic microangiopathy caused by dysregulation of the alternate complement pathway. It is characterized by renal involvement, but extrarenal involvement is common. Gastrointestinal (GI) complications, such as diarrhea, vomiting, GI bleeding, and inflammatory bowel disease (IBD) are common. However, isolated small bowel/colonic ulcerations in aHUS have not been reported. We present a challenging caseof small and large bowel ulcerations in aHUS.
Case Description/Methods: A 36-year-old woman with history of aHUS and secondary end stage renal disease on hemodialysis presented to our emergency department with a 3-month history of severe epigastric pain. She was initially treated with eculizumab loading followed by ravulizumab maintenancetherapy. She had several outside hospitalizations for abdominal pain, diarrhea and vomiting since her diagnosis. Workup included a non-contrast CT scan with terminal ileum (TI), cecal, and ascending colonic thickening. EGD and colonoscopy revealed small duodenal and TI ulcerations, but pathology showed nonspecific inflammation. She was treated with a short course of prednisone and budesonide with possibly mild improvement. On presentation to our center, she had epigastric pain and stable anemia without evidence of hemolysis. Enteroscopy and colonoscopy revealed deep large ulcers in the third and fourth portion of the duodenum, proximaljejunum, and one small superficial ulcer in the cecum. MRI showed mild thickening and hyperemia of jejunal loops. She was initially treated with IV steroids but had no clinical response this time. After review by multiple expert pathologists, it was determined that her ulcerationswere due to microvascular thrombi. Extensive hematologic, autoimmune and infectious workupsfor alternate etiologies were negative. Hematology restarted her on weekly eculizumab loading with significant improvement in her abdominal pain, and she was discharged with close hematology follow up.
Discussion: Intestinal ulcerations in aHUS can develop secondary to microvascular thrombosis and resultantischemia. IBD was considered, but the absence of chronic inflammatory changes on biopsy and lack of response to steroids argue against it. MRI and endoscopic evaluation are crucial for determining the etiology of small bowel ulcerations in aHUS patients. Treatment is primarily aimed at treating the underlying aHUS. To our knowledge, this is a very rare complication with no other cases found in the literature.

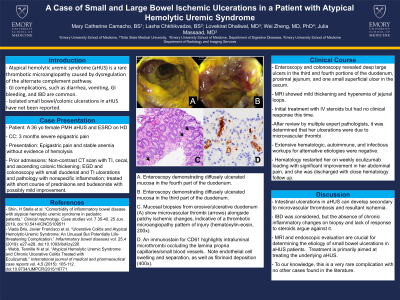
Figure: A. Enteroscopy demonstrating diffusely ulcerated mucosa in the fourth part of the duodenum.
B. Enteroscopy demonstrating diffusely ulcerated mucosa in the third part of the duodenum.
C. Mucosal biopsies from erosive/ulcerative duodenum (A) show microvascular thrombi (arrows) alongside patchy ischemic changes, indicative of a thrombotic microangiopathy pattern of injury (hematoxylin-eosin, 200x).
D. An immunostain for CD61 highlights intraluminal microthrombi occluding the lamina propria capillaries/small blood vessels. Note endothelial cell swelling and separation, as well as fibrinoid deposition (400x).
B. Enteroscopy demonstrating diffusely ulcerated mucosa in the third part of the duodenum.
C. Mucosal biopsies from erosive/ulcerative duodenum (A) show microvascular thrombi (arrows) alongside patchy ischemic changes, indicative of a thrombotic microangiopathy pattern of injury (hematoxylin-eosin, 200x).
D. An immunostain for CD61 highlights intraluminal microthrombi occluding the lamina propria capillaries/small blood vessels. Note endothelial cell swelling and separation, as well as fibrinoid deposition (400x).
Disclosures:
Mary Camacho indicated no relevant financial relationships.
Julia Massaad indicated no relevant financial relationships.
Lovekirat Dhaliwal indicated no relevant financial relationships.
Lasha Chkhikvadze indicated no relevant financial relationships.
Wei Zheng indicated no relevant financial relationships.
Mary Camacho, BS1, Julia Massaad, MD1, Lovekirat Dhaliwal, MD1, Lasha Chkhikvadze, 2, Wei Zheng, MD, PhD1. P1561 - A Case of Small and Large Bowel Ischemic Ulcerations in a Patient With Atypical Hemolytic Uremic Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
