Sunday Poster Session
Category: Small Intestine
P1565 - Unlocking the Digestive Dilemma: Sevelamer's Trail in Gastrointestinal Dysfunction and Literature Review
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Pujitha Vallivedu Chennakesavulu, MD, MBBS
Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center
Bridgeport, CT
Presenting Author(s)
Award: Presidential Poster Award
Pujitha Vallivedu Chennakesavulu, MD, MBBS, Sushrut Ingawale, MD, MBBS, Phanidhar Mogga, MD, MBBS, Prabin Sharma, MD
Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT
Introduction: Sevelamer is an anion-exchange resin used to treat hyperphosphatemia in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD). Sevelamer-induced gastrointestinal (GI) complications are characterized by erosions, inflammatory polyps, and circumferential ulcerations in specific segments of the large intestine, coupled with necrosis and ischemic alterations. Our case highlights the formation of sevelamer concretions in GI mucosa and explains the expectant diagnostics and management.
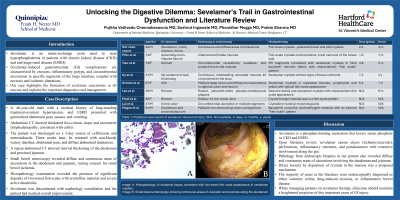
Case Description/Methods: A 46-year-old male with a medical history of long-standing treatment-resistant hypertension, and ESRD presented with generalized abdominal pain, nausea, and vomiting. Abdominal CT showed thickened ileo-colonic loops and mesenteric lymphadenopathy, consistent with colitis. The patient was discharged on a 5-day course of ceftriaxone and metronidazole. Three weeks later, he returned with non-bloody watery diarrhea, abdominal pain, and diffuse abdominal tenderness. A repeat abdominal CT showed interval thickening of the duodenum and proximal jejunum. Small bowel enteroscopy revealed diffuse and continuous areas of ulcerations in the duodenum and jejunum, raising concern for small bowel ischemia. Histopathology examination revealed the presence of significant deposits of two-toned fish scales with crystalline material and severe active duodenitis. Sevelamer was discontinued with nephrology consultation and the patient had marked overall improvement.
Discussion: Sevelamer is a phosphate-binding medication that lowers serum phosphate in CKD and ESRD. Upon literature review, sevelamer causes ulcers (ischemic/necrotic), perforations, inflammatory strictures, and pseudotumors with extensive involvement along the gut. Similar to the reports in the table (Table 1), pathology from endoscopic biopsies in our patient also revealed diffuse and continuous areas of ulcerations involving the duodenum and jejunum. Direct toxicity by deposition of crystals in the mucosa was a proposed mechanism. The majority of cases in the literature were endoscopically diagnosed as either ischemic colitis, drug-induced erosions, or inflammatory bowel disease. Our patient’s clinical history and morphological identification of sevelamer crystals with a fish scale appearance were essential in confirming the diagnosis. While managing patients on sevelamer therapy, clinicians should maintain a heightened suspicion of this important cause of GI injury.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pujitha Vallivedu Chennakesavulu, MD, MBBS, Sushrut Ingawale, MD, MBBS, Phanidhar Mogga, MD, MBBS, Prabin Sharma, MD. P1565 - Unlocking the Digestive Dilemma: Sevelamer's Trail in Gastrointestinal Dysfunction and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Pujitha Vallivedu Chennakesavulu, MD, MBBS, Sushrut Ingawale, MD, MBBS, Phanidhar Mogga, MD, MBBS, Prabin Sharma, MD
Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT
Introduction: Sevelamer is an anion-exchange resin used to treat hyperphosphatemia in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD). Sevelamer-induced gastrointestinal (GI) complications are characterized by erosions, inflammatory polyps, and circumferential ulcerations in specific segments of the large intestine, coupled with necrosis and ischemic alterations. Our case highlights the formation of sevelamer concretions in GI mucosa and explains the expectant diagnostics and management.
Case Description/Methods: A 46-year-old male with a medical history of long-standing treatment-resistant hypertension, and ESRD presented with generalized abdominal pain, nausea, and vomiting. Abdominal CT showed thickened ileo-colonic loops and mesenteric lymphadenopathy, consistent with colitis. The patient was discharged on a 5-day course of ceftriaxone and metronidazole. Three weeks later, he returned with non-bloody watery diarrhea, abdominal pain, and diffuse abdominal tenderness. A repeat abdominal CT showed interval thickening of the duodenum and proximal jejunum. Small bowel enteroscopy revealed diffuse and continuous areas of ulcerations in the duodenum and jejunum, raising concern for small bowel ischemia. Histopathology examination revealed the presence of significant deposits of two-toned fish scales with crystalline material and severe active duodenitis. Sevelamer was discontinued with nephrology consultation and the patient had marked overall improvement.
Discussion: Sevelamer is a phosphate-binding medication that lowers serum phosphate in CKD and ESRD. Upon literature review, sevelamer causes ulcers (ischemic/necrotic), perforations, inflammatory strictures, and pseudotumors with extensive involvement along the gut. Similar to the reports in the table (Table 1), pathology from endoscopic biopsies in our patient also revealed diffuse and continuous areas of ulcerations involving the duodenum and jejunum. Direct toxicity by deposition of crystals in the mucosa was a proposed mechanism. The majority of cases in the literature were endoscopically diagnosed as either ischemic colitis, drug-induced erosions, or inflammatory bowel disease. Our patient’s clinical history and morphological identification of sevelamer crystals with a fish scale appearance were essential in confirming the diagnosis. While managing patients on sevelamer therapy, clinicians should maintain a heightened suspicion of this important cause of GI injury.

Figure: Image A: Histopathology of duodenal biopsy consistent with two-toned fish scale appearance of sevelamer crystals; Image B: Small bowel enteroscopy showing continuous areas of ulceration and necrosis along the duodenum
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Pujitha Vallivedu Chennakesavulu indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Phanidhar Mogga indicated no relevant financial relationships.
Prabin Sharma indicated no relevant financial relationships.
Pujitha Vallivedu Chennakesavulu, MD, MBBS, Sushrut Ingawale, MD, MBBS, Phanidhar Mogga, MD, MBBS, Prabin Sharma, MD. P1565 - Unlocking the Digestive Dilemma: Sevelamer's Trail in Gastrointestinal Dysfunction and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

