Sunday Poster Session
Category: Small Intestine
P1575 - Undercover Ulcers: The Misleading Presentation of Duodenal Bulb Perforation as Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Taha Bin Arif, MBBS, MD
Sinai Hospital
Baltimore, MD
Presenting Author(s)
Taha Bin Arif, MBBS, MD1, Harika Davuluri, MBBS, MD1, Chiranjeevi Sainatham, MBBS, MD1, Asad Ur Rahman, MD2, Muhammad Zarrar Khan, MD3
1Sinai Hospital, Baltimore, MD; 2Cleveland Clinic Florida, Weston, FL; 3Henry Ford Hospital, Royal Oak, MI
Introduction: Duodenal ulcers and acute pancreatitis (AP) are common gastrointestinal diseases. AP can result from various factors, including cholelithiasis and alcoholism, and, rarely, from duodenal ulcer perforation (DIP). We report an 83-year-old woman with AP due to a large duodenal ulcer perforation extending into the pancreas, requiring emergent surgery.
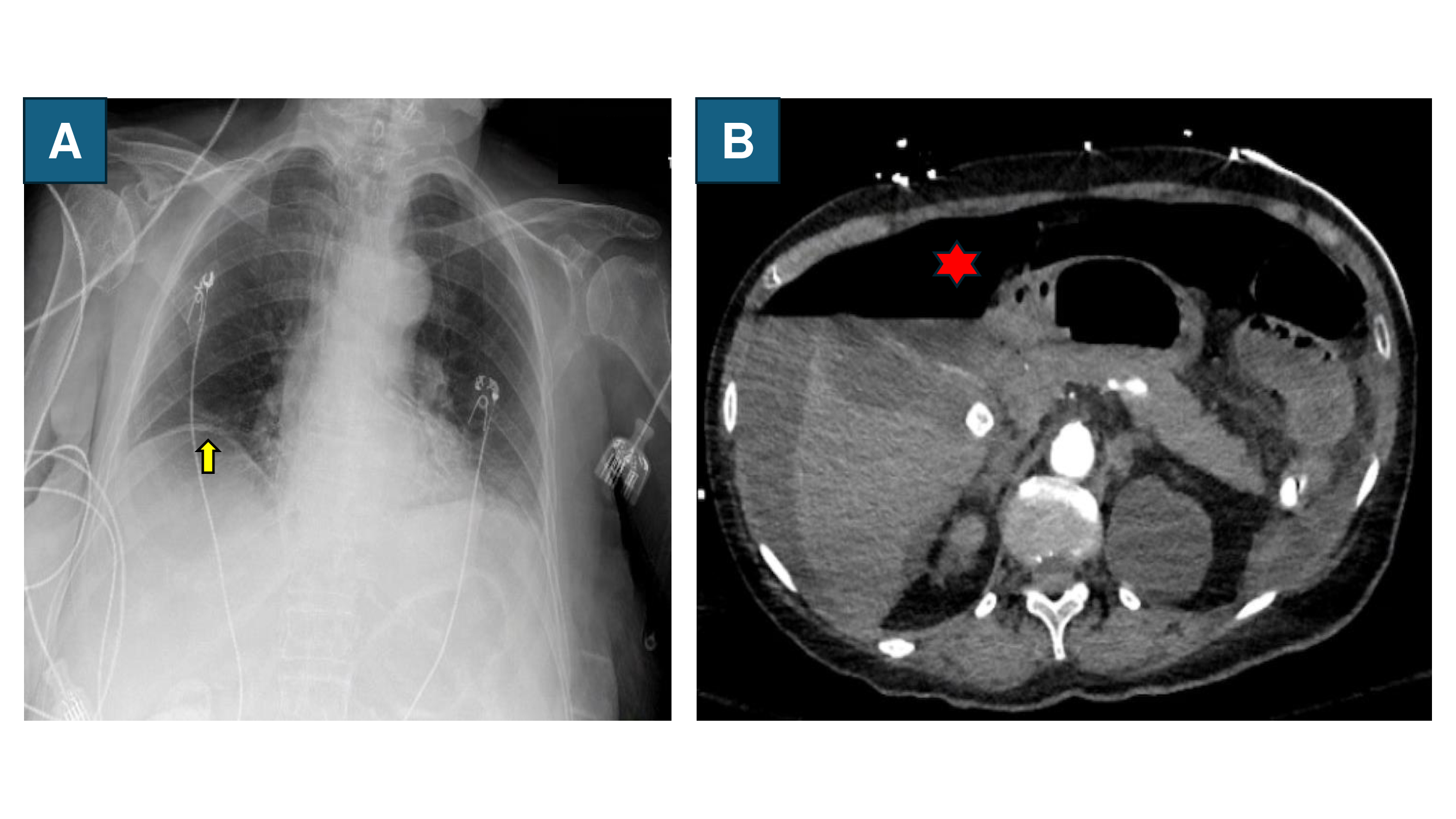
Case Description/Methods: An 83-year-old female with Alzheimer’s disease, osteoarthritis, and hypertension presented with worsening abdominal pain over 2-3 weeks, with no associated symptoms. Her home medications included aspirin, lisinopril, meloxicam, and donepezil. On presentation, she displayed normal vital signs. Physical examination revealed signs of dehydration and asthenia, with right upper quadrant and epigastric tenderness. Laboratory results indicated hyponatremia, elevated BUN and creatinine, anion gap metabolic acidosis, elevated lipase (1263 U/L), and leukopenia. An EKG showed sinus tachycardia. Intravenous fluids, morphine, bowel rest, and pantoprazole were started considering it as a case of AP. A CT abdomen with contrast could not be performed initially due to acute kidney injury. Abdominal ultrasound revealed cholelithiasis without cholecystitis. Eventually, the patient developed hypoxia and was put on 4L oxygen. A chest X-ray revealed air under the diaphragm, prompting urgent surgical consultation. The patient went into cardiac arrest shortly but was successfully resuscitated. Following intubation, a CT scan revealed free intraperitoneal air, leading to an urgent exploratory laparotomy. A 4 cm perforation was seen in the duodenal bulb with erosion into the anterior pancreas. Antrectomy and Roux-en-Y gastrojejunostomy were performed. Post-surgery, she was administered antibiotics resulting in improved lactate and lipase levels.
Discussion: In this case, our patient initially presented with vague AP symptoms like epigastric pain, lethargy, and anorexia. Her rapid respiratory decline led to a chest X-ray, revealing air under the diaphragm. This case shows that physical exams can be nonspecific for DUP causing AP, especially in older adults. DUP should be considered in acute epigastric pain, particularly in patients with a history or risk factors of PUD (e.g., NSAID use for osteoarthritis). Her renal dysfunction delayed a CT scan and the DUP diagnosis that led to her decompensation. Therefore, it is crucial to rule out PUD in adults with risk factors when no clear trigger for AP is found to prevent morbidity and mortality.
Disclosures:
Taha Bin Arif, MBBS, MD1, Harika Davuluri, MBBS, MD1, Chiranjeevi Sainatham, MBBS, MD1, Asad Ur Rahman, MD2, Muhammad Zarrar Khan, MD3. P1575 - Undercover Ulcers: The Misleading Presentation of Duodenal Bulb Perforation as Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Sinai Hospital, Baltimore, MD; 2Cleveland Clinic Florida, Weston, FL; 3Henry Ford Hospital, Royal Oak, MI
Introduction: Duodenal ulcers and acute pancreatitis (AP) are common gastrointestinal diseases. AP can result from various factors, including cholelithiasis and alcoholism, and, rarely, from duodenal ulcer perforation (DIP). We report an 83-year-old woman with AP due to a large duodenal ulcer perforation extending into the pancreas, requiring emergent surgery.
Case Description/Methods: An 83-year-old female with Alzheimer’s disease, osteoarthritis, and hypertension presented with worsening abdominal pain over 2-3 weeks, with no associated symptoms. Her home medications included aspirin, lisinopril, meloxicam, and donepezil. On presentation, she displayed normal vital signs. Physical examination revealed signs of dehydration and asthenia, with right upper quadrant and epigastric tenderness. Laboratory results indicated hyponatremia, elevated BUN and creatinine, anion gap metabolic acidosis, elevated lipase (1263 U/L), and leukopenia. An EKG showed sinus tachycardia. Intravenous fluids, morphine, bowel rest, and pantoprazole were started considering it as a case of AP. A CT abdomen with contrast could not be performed initially due to acute kidney injury. Abdominal ultrasound revealed cholelithiasis without cholecystitis. Eventually, the patient developed hypoxia and was put on 4L oxygen. A chest X-ray revealed air under the diaphragm, prompting urgent surgical consultation. The patient went into cardiac arrest shortly but was successfully resuscitated. Following intubation, a CT scan revealed free intraperitoneal air, leading to an urgent exploratory laparotomy. A 4 cm perforation was seen in the duodenal bulb with erosion into the anterior pancreas. Antrectomy and Roux-en-Y gastrojejunostomy were performed. Post-surgery, she was administered antibiotics resulting in improved lactate and lipase levels.
Discussion: In this case, our patient initially presented with vague AP symptoms like epigastric pain, lethargy, and anorexia. Her rapid respiratory decline led to a chest X-ray, revealing air under the diaphragm. This case shows that physical exams can be nonspecific for DUP causing AP, especially in older adults. DUP should be considered in acute epigastric pain, particularly in patients with a history or risk factors of PUD (e.g., NSAID use for osteoarthritis). Her renal dysfunction delayed a CT scan and the DUP diagnosis that led to her decompensation. Therefore, it is crucial to rule out PUD in adults with risk factors when no clear trigger for AP is found to prevent morbidity and mortality.
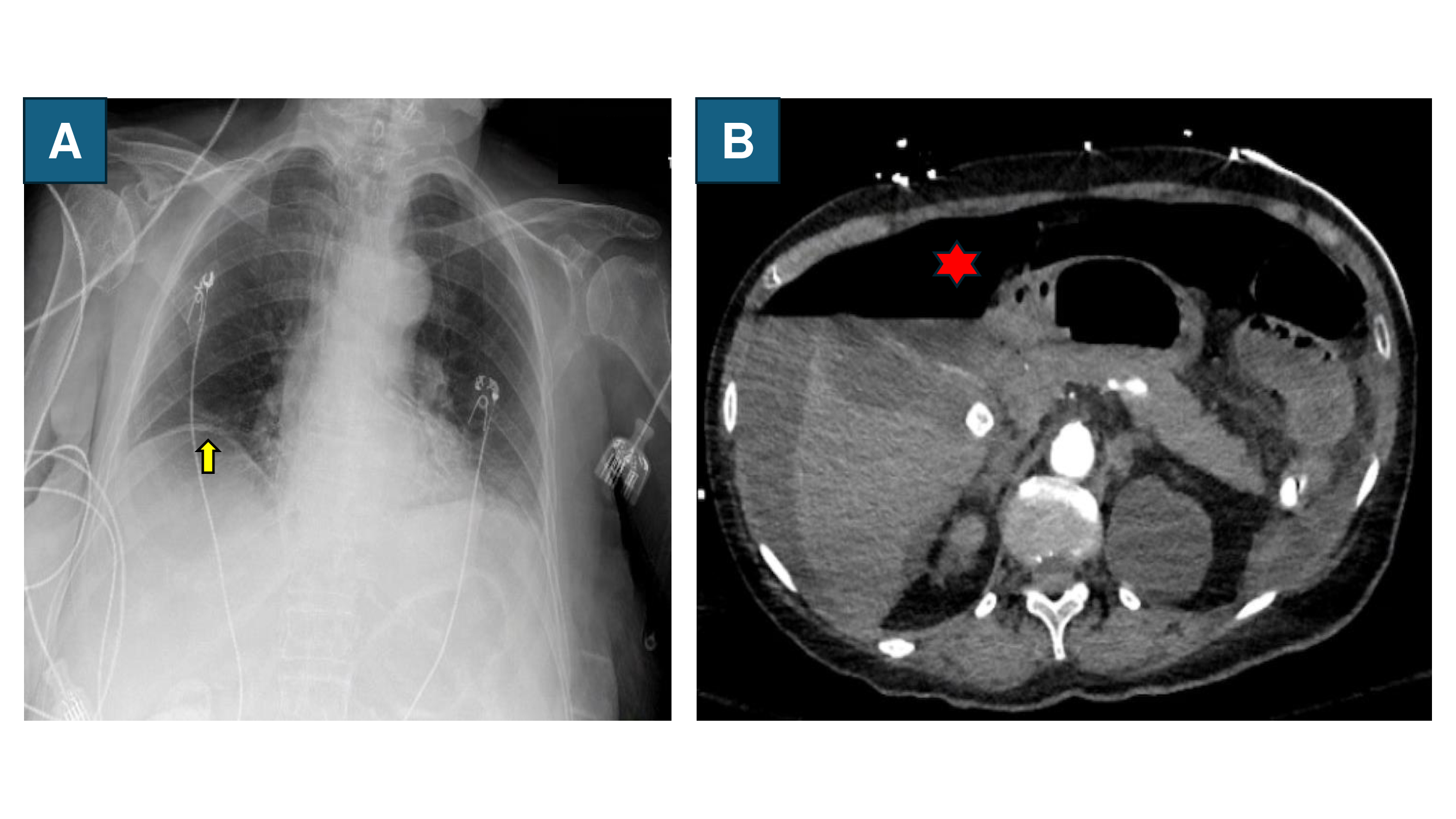
Figure: Figure A: Chest Xray demonstrating air under diaphragm (yellow arrow). Figure B: CT scan of abdomen with contrast showing large amount of free intraperitoneal air and moderately large amount of ascites adjacent to the liver (red star).
Disclosures:
Taha Bin Arif indicated no relevant financial relationships.
Harika Davuluri indicated no relevant financial relationships.
Chiranjeevi Sainatham indicated no relevant financial relationships.
Asad Ur Rahman: Abbvie – Speakers Bureau.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Taha Bin Arif, MBBS, MD1, Harika Davuluri, MBBS, MD1, Chiranjeevi Sainatham, MBBS, MD1, Asad Ur Rahman, MD2, Muhammad Zarrar Khan, MD3. P1575 - Undercover Ulcers: The Misleading Presentation of Duodenal Bulb Perforation as Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
