Sunday Poster Session
Category: Stomach
P1608 - Racial And Gender Disparities In GIM Improvement With PPI Treatment: A Comprehensive Analysis Using Inhouse Database From 2009-2023
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

- RR
Rajmohan Rammohan, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA
Nassau University Medical Center, East Meadow, NY
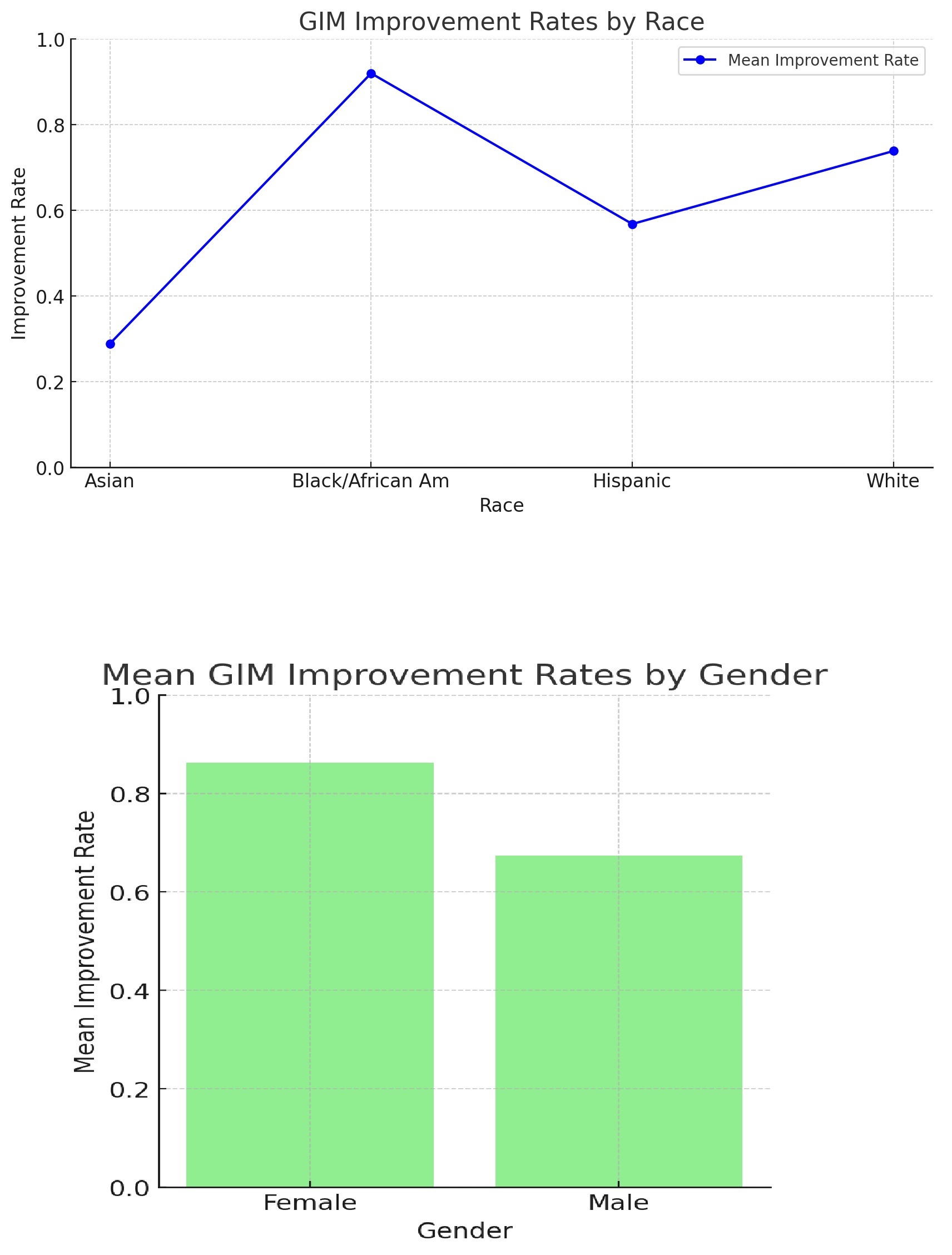
Introduction: Proton pump inhibitors (PPIs) are widely used to treat gastrointestinal disorders, including gastric intestinal metaplasia (GIM), a precancerous condition marked by abnormal stomach lining changes, raising gastric cancer risk. This study evaluates PPI effectiveness in improving GIM across racial groups, focusing on disparities among Asians, Black/African Americans, Hispanics, and Whites. By analyzing post-treatment GIM status, we aim to understand how racial and gender differences impact PPI therapy efficacy and inform tailored treatment for diverse populations
Methods: The study examined 4300 patients with Gastric Intestinal Metaplasia from 2009-2023, with 377 undergoing repeat endoscopies after ≥ 8 weeks of PPI therapy. Chi-square tests evaluated PPI's impact on GIM status, considering post-treatment status, race, and gender. The primary analysis compared GIM improvement post-8-week PPI treatment. Secondary analyses assessed improvement across races (Asian, Black/African American, Hispanic, White) and genders. P-values determined statistical significance.
Results: The study population included males and females from diverse racial backgrounds. Asian, Black/African American, Hispanic, and White. Among the participants, the gender distribution was 40% female and 60% male. Racially, the population comprised 10% Asian, 50% Black/African American, 15% Hispanic, and 25% White. Results indicate significant improvement with PPI (Chi2 = 13.12, p = 0.0003). Significant racial disparities were observed (Chi2 = 165.48, p = 0.0000), with Black/African Americans exhibiting the most improvement. Moreover, a gender difference was noted (Chi2 = 22.03, p = 0.0000026), favoring females
Discussion: The study reveals significant PPI-induced GIM improvement, with notable racial and gender disparities. Black/African Americans exhibit the most substantial enhancement, possibly due to genetic or environmental factors. Females also show greater improvement, suggesting hormonal or behavioral influences. These findings emphasize personalized GIM management, considering racial and gender variations for optimal outcomes. Further research is essential to unravel underlying mechanisms and develop targeted interventions ensuring equitable healthcare benefits. This study lays a critical groundwork for reducing gastric cancer risks via effective GIM management with PPI therapy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P1608 - Racial And Gender Disparities In GIM Improvement With PPI Treatment: A Comprehensive Analysis Using Inhouse Database From 2009-2023, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Proton pump inhibitors (PPIs) are widely used to treat gastrointestinal disorders, including gastric intestinal metaplasia (GIM), a precancerous condition marked by abnormal stomach lining changes, raising gastric cancer risk. This study evaluates PPI effectiveness in improving GIM across racial groups, focusing on disparities among Asians, Black/African Americans, Hispanics, and Whites. By analyzing post-treatment GIM status, we aim to understand how racial and gender differences impact PPI therapy efficacy and inform tailored treatment for diverse populations
Methods: The study examined 4300 patients with Gastric Intestinal Metaplasia from 2009-2023, with 377 undergoing repeat endoscopies after ≥ 8 weeks of PPI therapy. Chi-square tests evaluated PPI's impact on GIM status, considering post-treatment status, race, and gender. The primary analysis compared GIM improvement post-8-week PPI treatment. Secondary analyses assessed improvement across races (Asian, Black/African American, Hispanic, White) and genders. P-values determined statistical significance.
Results: The study population included males and females from diverse racial backgrounds. Asian, Black/African American, Hispanic, and White. Among the participants, the gender distribution was 40% female and 60% male. Racially, the population comprised 10% Asian, 50% Black/African American, 15% Hispanic, and 25% White. Results indicate significant improvement with PPI (Chi2 = 13.12, p = 0.0003). Significant racial disparities were observed (Chi2 = 165.48, p = 0.0000), with Black/African Americans exhibiting the most improvement. Moreover, a gender difference was noted (Chi2 = 22.03, p = 0.0000026), favoring females
Discussion: The study reveals significant PPI-induced GIM improvement, with notable racial and gender disparities. Black/African Americans exhibit the most substantial enhancement, possibly due to genetic or environmental factors. Females also show greater improvement, suggesting hormonal or behavioral influences. These findings emphasize personalized GIM management, considering racial and gender variations for optimal outcomes. Further research is essential to unravel underlying mechanisms and develop targeted interventions ensuring equitable healthcare benefits. This study lays a critical groundwork for reducing gastric cancer risks via effective GIM management with PPI therapy.
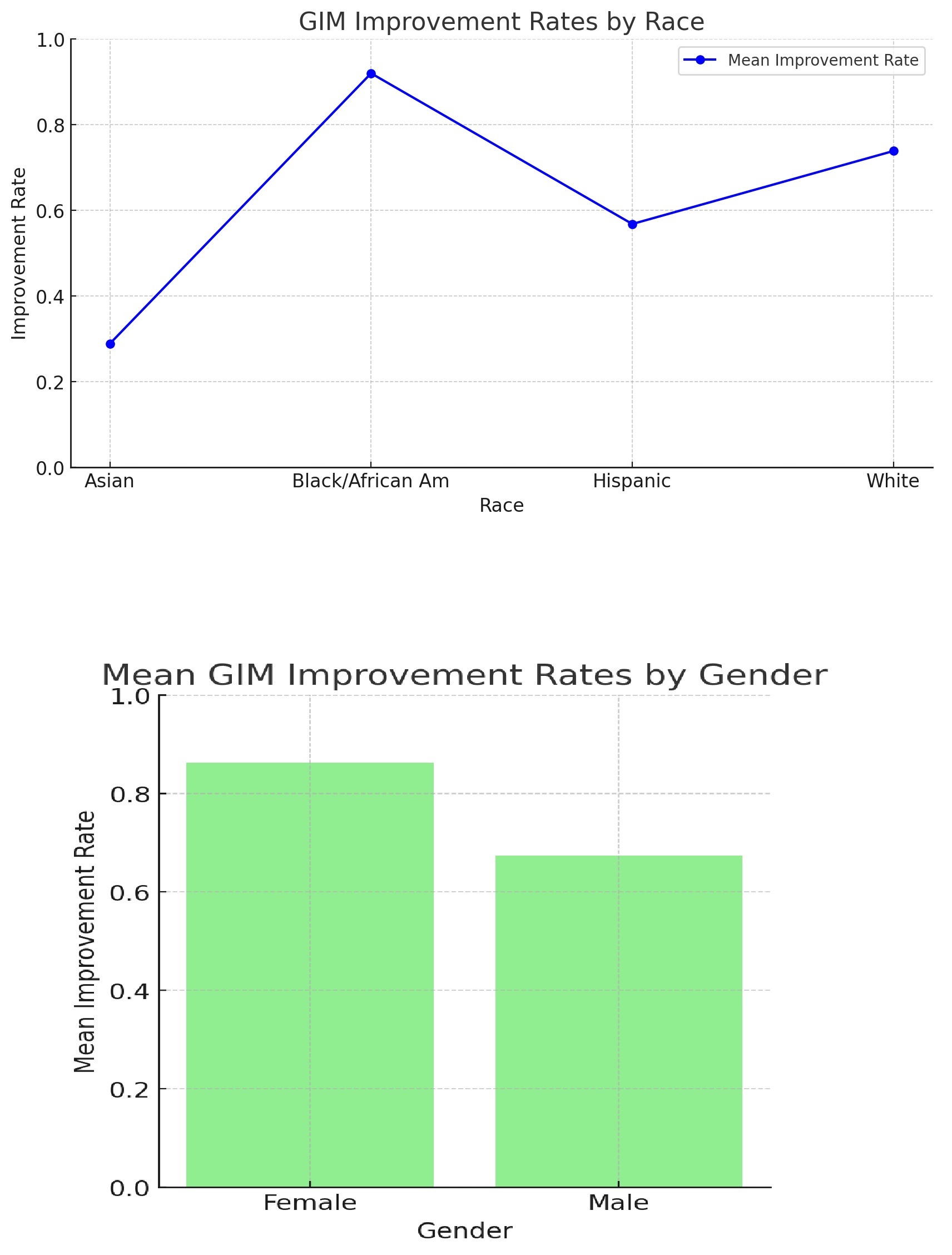
Figure: Relationship between PPI treatment and Gastric Intestinal Metaplasia
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Mohan Ram Mohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Sai Greeshma Magam indicated no relevant financial relationships.
Melvin Joy indicated no relevant financial relationships.
Dilman Natt indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Winghang Lau indicated no relevant financial relationships.
Abhishek Tadikonda indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Krishnaiyer Subramani indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P1608 - Racial And Gender Disparities In GIM Improvement With PPI Treatment: A Comprehensive Analysis Using Inhouse Database From 2009-2023, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
