Sunday Poster Session
Category: Stomach
P1638 - A Case of Immune Checkpoint Inhibitor-Associated Gastritis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Mahmoud Mansour, MD
University of Missouri Health Care
Columbia, MO
Presenting Author(s)
Mahmoud Mansour, MD1, Mohammad Abudalou, MBBS1, Hanna Nale, MD1, Deepthi Rao, MD, MS2, Ghassan Hammoud, MD1
1University of Missouri Health Care, Columbia, MO; 2University of Missouri School of Medicine, Columbia, MO
Introduction: Immune checkpoint inhibitors (ICIs) are a cornerstone in cancer therapy, offering significant benefits but also presenting risks, notably immune-related adverse events (irAEs). Among these, irAE gastritis, poses challenges due to its rarity and non-specific symptoms, requiring diligent diagnosis through combined clinical, endoscopic, and histopathological evaluation.
Case Description/Methods: A 52-year-old woman diagnosed with Stage IIIB endometrioid carcinoma of the uterus presented with persistent nausea and vomiting. Her previous treatment included chemotherapy with Carboplatin and Taxol, surgery, radiation, and she recently completed the seventh cycle of a 14-cycle Keytruda maintenance course.
The symptoms began four weeks before hospitalization, consisting of daily non-bloody vomiting and constant epigastric pain. She noted a weight loss of about 20 pounds over 2.5 months, without diarrhea, rectal bleeding, or hematemesis.
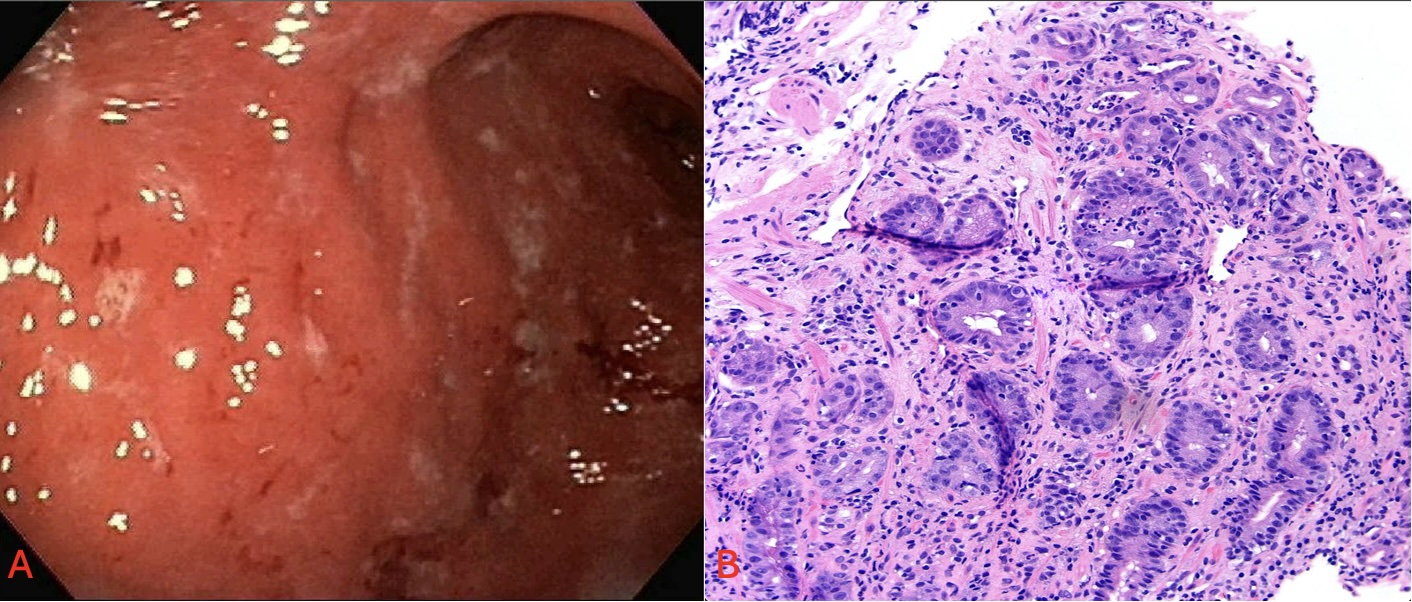
On admission, an MRI of her abdomen and pelvis showed signs of gastritis but no tumor recurrence or spread. EGD revealed moderate to severe gastric erythema, edema, and atrophy of the mucosal folds with superficial erosions (Figure). Biopsies showed chronic active gastritis with increased lymphocytes and apoptotic activity (Figure), suggesting a diagnosis of gastritis due to immune checkpoint inhibitor therapy.
Treatment started with 25mg (0.5 mg/kg) of prednisolone daily, to be reduced by 5 mg weekly after two weeks. Her condition improved markedly within three days of starting steroids. She was discharged, reported complete symptom resolution after two weeks, and progressed to a regular diet without issues.
Discussion: ICIs primarily activate effector T cells by inhibiting PD-1, PD-L1, and CTLA-4, potentially leading to irAEs due to increased cytokine production and reduced self-tolerance. Endoscopic examinations often show antrum-predominant erosions, erythematous and edematous mucosa with purulent discharge, and highly fragile mucosa that bleeds easily. Histologically, features such as diffuse, active chronic gastritis with increased intraepithelial lymphocytes and apoptotic activity are common. Treatment typically starts with corticosteroids, which can quickly alleviate symptoms. For cases resistant to steroids, therapies such as anti-TNFα monoclonal antibodies are considered.
Disclosures:
Mahmoud Mansour, MD1, Mohammad Abudalou, MBBS1, Hanna Nale, MD1, Deepthi Rao, MD, MS2, Ghassan Hammoud, MD1. P1638 - A Case of Immune Checkpoint Inhibitor-Associated Gastritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri Health Care, Columbia, MO; 2University of Missouri School of Medicine, Columbia, MO
Introduction: Immune checkpoint inhibitors (ICIs) are a cornerstone in cancer therapy, offering significant benefits but also presenting risks, notably immune-related adverse events (irAEs). Among these, irAE gastritis, poses challenges due to its rarity and non-specific symptoms, requiring diligent diagnosis through combined clinical, endoscopic, and histopathological evaluation.
Case Description/Methods: A 52-year-old woman diagnosed with Stage IIIB endometrioid carcinoma of the uterus presented with persistent nausea and vomiting. Her previous treatment included chemotherapy with Carboplatin and Taxol, surgery, radiation, and she recently completed the seventh cycle of a 14-cycle Keytruda maintenance course.
The symptoms began four weeks before hospitalization, consisting of daily non-bloody vomiting and constant epigastric pain. She noted a weight loss of about 20 pounds over 2.5 months, without diarrhea, rectal bleeding, or hematemesis.
On admission, an MRI of her abdomen and pelvis showed signs of gastritis but no tumor recurrence or spread. EGD revealed moderate to severe gastric erythema, edema, and atrophy of the mucosal folds with superficial erosions (Figure). Biopsies showed chronic active gastritis with increased lymphocytes and apoptotic activity (Figure), suggesting a diagnosis of gastritis due to immune checkpoint inhibitor therapy.
Treatment started with 25mg (0.5 mg/kg) of prednisolone daily, to be reduced by 5 mg weekly after two weeks. Her condition improved markedly within three days of starting steroids. She was discharged, reported complete symptom resolution after two weeks, and progressed to a regular diet without issues.
Discussion: ICIs primarily activate effector T cells by inhibiting PD-1, PD-L1, and CTLA-4, potentially leading to irAEs due to increased cytokine production and reduced self-tolerance. Endoscopic examinations often show antrum-predominant erosions, erythematous and edematous mucosa with purulent discharge, and highly fragile mucosa that bleeds easily. Histologically, features such as diffuse, active chronic gastritis with increased intraepithelial lymphocytes and apoptotic activity are common. Treatment typically starts with corticosteroids, which can quickly alleviate symptoms. For cases resistant to steroids, therapies such as anti-TNFα monoclonal antibodies are considered.
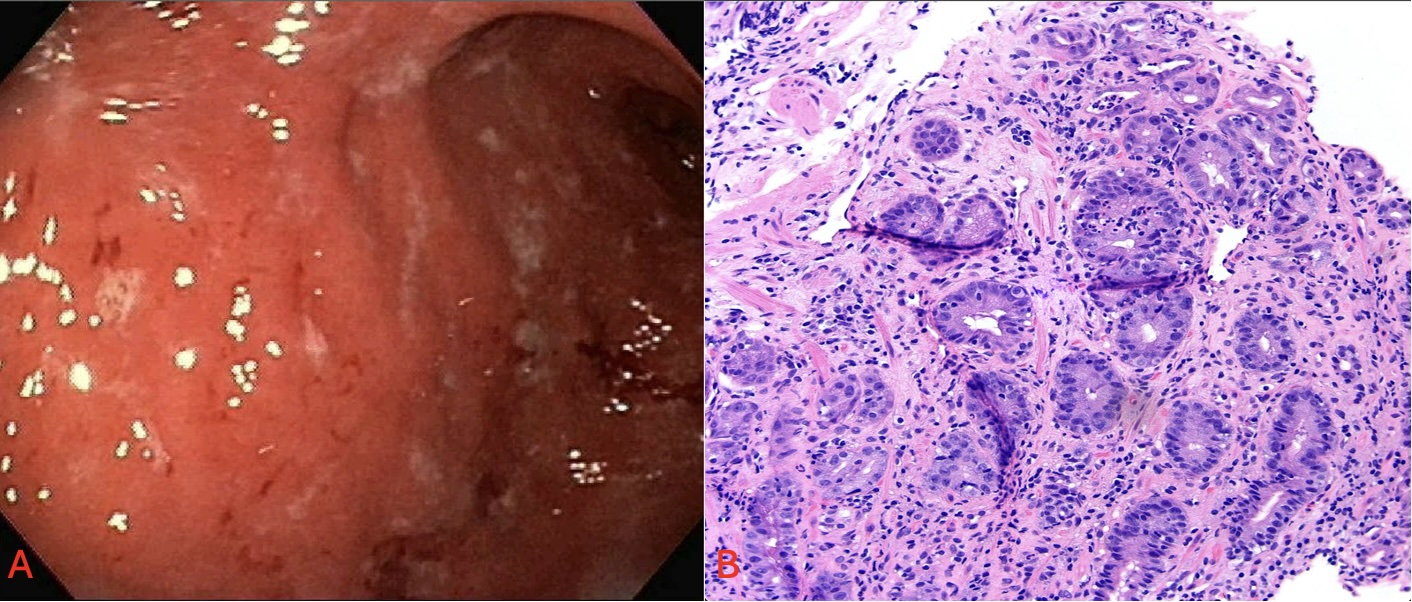
Figure: A: Endoscopic view showing gastric erythema, edema, and atrophy of the mucosal folds with superficial erosions. B: Hematoxylin and eosin stain 20X, showing lymphoplasmocytic infiltrates along with cryptitis with abscesses
Disclosures:
Mahmoud Mansour indicated no relevant financial relationships.
Mohammad Abudalou indicated no relevant financial relationships.
Hanna Nale indicated no relevant financial relationships.
Deepthi Rao indicated no relevant financial relationships.
Ghassan Hammoud indicated no relevant financial relationships.
Mahmoud Mansour, MD1, Mohammad Abudalou, MBBS1, Hanna Nale, MD1, Deepthi Rao, MD, MS2, Ghassan Hammoud, MD1. P1638 - A Case of Immune Checkpoint Inhibitor-Associated Gastritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
