Sunday Poster Session
Category: Stomach
P1640 - Air Coli: An Ominous Imaging Finding of Acute Gastroenteritis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- CA
Chima Amadi, MD, MBA
Morehouse School of Medicine
Atlanta, GA
Presenting Author(s)
Chima Amadi, MD, MBA1, Brittany S. Tummings, MD1, Aaron M. Hein, MD2, Brian Curtis, MD3, Sara Levy, MD4
1Morehouse School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Tucker, GA; 3VHA National Teleradiology Program, Palo Alto, CA; 4Emory University, Atlanta, GA
Introduction: Gastric pneumatosis (GP) is a rare clinical entity often associated with a poor prognosis. We present a case of presumably infectious GP on short-interval imaging, which was successfully managed conservatively.
Case Description/Methods: A 75-year-old male with a past medical history significant for advanced dementia and hypertension presented with 7 days of nausea, vomiting, and non-bloody diarrhea, with subsequent lethargy for 2 days. Initially, the exam was notable for acute encephalopathy, tachycardia, and a distended tympanic abdomen. Lab results showed a 10.3k/mcL white blood cell count, 2.6mmol/L lactic acid, and 11gm/dL hemoglobin. After resuscitation, the patient developed coffee-ground emesis and atrial fibrillation.
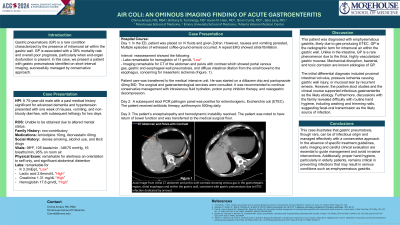
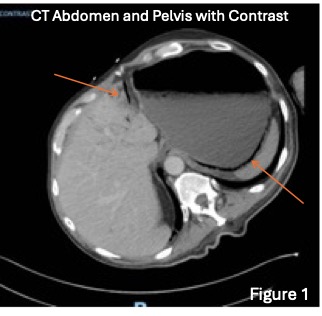
CT of the abdomen and pelvis with contrast noted portal venous gas, gastric and esophageal wall pneumatosis, and diffuse intestinal dilation from the small bowel to the esophagus, which is concerning for mesenteric ischemia (Fig. 1). After surgical and gastroenterological consultation, conservative management with fluids, proton pump inhibitor therapy, and gastric decompression was pursued.
A subsequent stool PCR pathogen panel was positive for enterotoxigenic Escherichia coli (ETEC), and the patient received antibiotic therapy with subsequent improved mental and hemodynamic status, with the return of bowel function.
Discussion: This patient was diagnosed with emphysematous gastritis, likely due to gas-producing ETEC. GP is the radiographic term for intramural air within the gastric wall. Unlike in the intestine, GP is a rare phenomenon due to the thick, highly vascularized gastric mucosa. Mechanical disruption, bacterial, and toxic corrosion are known etiologies of GP. Our initial differential diagnosis included proximal intestinal volvulus, pressure ischemia causing gastric wall injury, or mucosal tear by recurrent emesis. However, the positive stool studies and the clinical course supported infectious gastroenteritis.
GP lacks specific treatment guidelines and can be managed conservatively or surgically. Antibiotic therapy, fluid resuscitation, parenteral nutrition, and gastric decompression are the accepted approaches to management, as early surgical intervention has been shown to increase postoperative complications. Surgical indications include bowel perforation, strictures, obstruction, or sepsis. This case highlights the importance of early CT imaging detection and the role of early conservative management strategies in successfully treating emphysematous gastritis.
Disclosures:
Chima Amadi, MD, MBA1, Brittany S. Tummings, MD1, Aaron M. Hein, MD2, Brian Curtis, MD3, Sara Levy, MD4. P1640 - Air Coli: An Ominous Imaging Finding of Acute Gastroenteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Morehouse School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Tucker, GA; 3VHA National Teleradiology Program, Palo Alto, CA; 4Emory University, Atlanta, GA
Introduction: Gastric pneumatosis (GP) is a rare clinical entity often associated with a poor prognosis. We present a case of presumably infectious GP on short-interval imaging, which was successfully managed conservatively.
Case Description/Methods: A 75-year-old male with a past medical history significant for advanced dementia and hypertension presented with 7 days of nausea, vomiting, and non-bloody diarrhea, with subsequent lethargy for 2 days. Initially, the exam was notable for acute encephalopathy, tachycardia, and a distended tympanic abdomen. Lab results showed a 10.3k/mcL white blood cell count, 2.6mmol/L lactic acid, and 11gm/dL hemoglobin. After resuscitation, the patient developed coffee-ground emesis and atrial fibrillation.
CT of the abdomen and pelvis with contrast noted portal venous gas, gastric and esophageal wall pneumatosis, and diffuse intestinal dilation from the small bowel to the esophagus, which is concerning for mesenteric ischemia (Fig. 1). After surgical and gastroenterological consultation, conservative management with fluids, proton pump inhibitor therapy, and gastric decompression was pursued.
A subsequent stool PCR pathogen panel was positive for enterotoxigenic Escherichia coli (ETEC), and the patient received antibiotic therapy with subsequent improved mental and hemodynamic status, with the return of bowel function.
Discussion: This patient was diagnosed with emphysematous gastritis, likely due to gas-producing ETEC. GP is the radiographic term for intramural air within the gastric wall. Unlike in the intestine, GP is a rare phenomenon due to the thick, highly vascularized gastric mucosa. Mechanical disruption, bacterial, and toxic corrosion are known etiologies of GP. Our initial differential diagnosis included proximal intestinal volvulus, pressure ischemia causing gastric wall injury, or mucosal tear by recurrent emesis. However, the positive stool studies and the clinical course supported infectious gastroenteritis.
GP lacks specific treatment guidelines and can be managed conservatively or surgically. Antibiotic therapy, fluid resuscitation, parenteral nutrition, and gastric decompression are the accepted approaches to management, as early surgical intervention has been shown to increase postoperative complications. Surgical indications include bowel perforation, strictures, obstruction, or sepsis. This case highlights the importance of early CT imaging detection and the role of early conservative management strategies in successfully treating emphysematous gastritis.
Figure: Axial image from initial CT abdomen and pelvis with contrast showing venous gas in the gastrohepatic region and within the gastric wall, consistent with gastric pneumatosis due to ETEC infection (indicated by arrows).
Disclosures:
Chima Amadi indicated no relevant financial relationships.
Brittany Tummings indicated no relevant financial relationships.
Aaron Hein indicated no relevant financial relationships.
Brian Curtis indicated no relevant financial relationships.
Sara Levy indicated no relevant financial relationships.
Chima Amadi, MD, MBA1, Brittany S. Tummings, MD1, Aaron M. Hein, MD2, Brian Curtis, MD3, Sara Levy, MD4. P1640 - Air Coli: An Ominous Imaging Finding of Acute Gastroenteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
