Sunday Poster Session
Category: Stomach
P1644 - Gastric Amyloidosis: A Rare Case of Melena and Hematemesis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AS
Andrea Schneider, DO
HonorHealth
Phoenix, AZ
Presenting Author(s)
Andrea Schneider, DO1, Mehul Patel, DO2, Joseph Fares, MD3, Gavin Levinthal, MD3, Bassel Al-Lahham, MD1
1HonorHealth, Phoenix, AZ; 2Honor Health Gastroenterology, Phoenix, AZ; 3HonorHealth, Scottsdale, AZ
Introduction: AL amyloidosis is a rare disorder caused by a clonal expansion of bone marrow plasma cells that secrete a monoclonal immunoglobulin light chain depositing as amyloid fibrils in tissues. 15% of these patients will have multiple myeloma. Although AL amyloid it is the most common type of amyloid seen, it is a rare condition, with an incidence of 9-14 cases per million and prevalence of 40.5 cases per million. Gastrointestinal bleeding due to amyloid deposition is infrequent. We describe a rare case of upper gastrointestinal bleeding that ultimately led to the diagnosis of GI amyloidosis in a patient who was recently diagnosed with multiple myeloma.
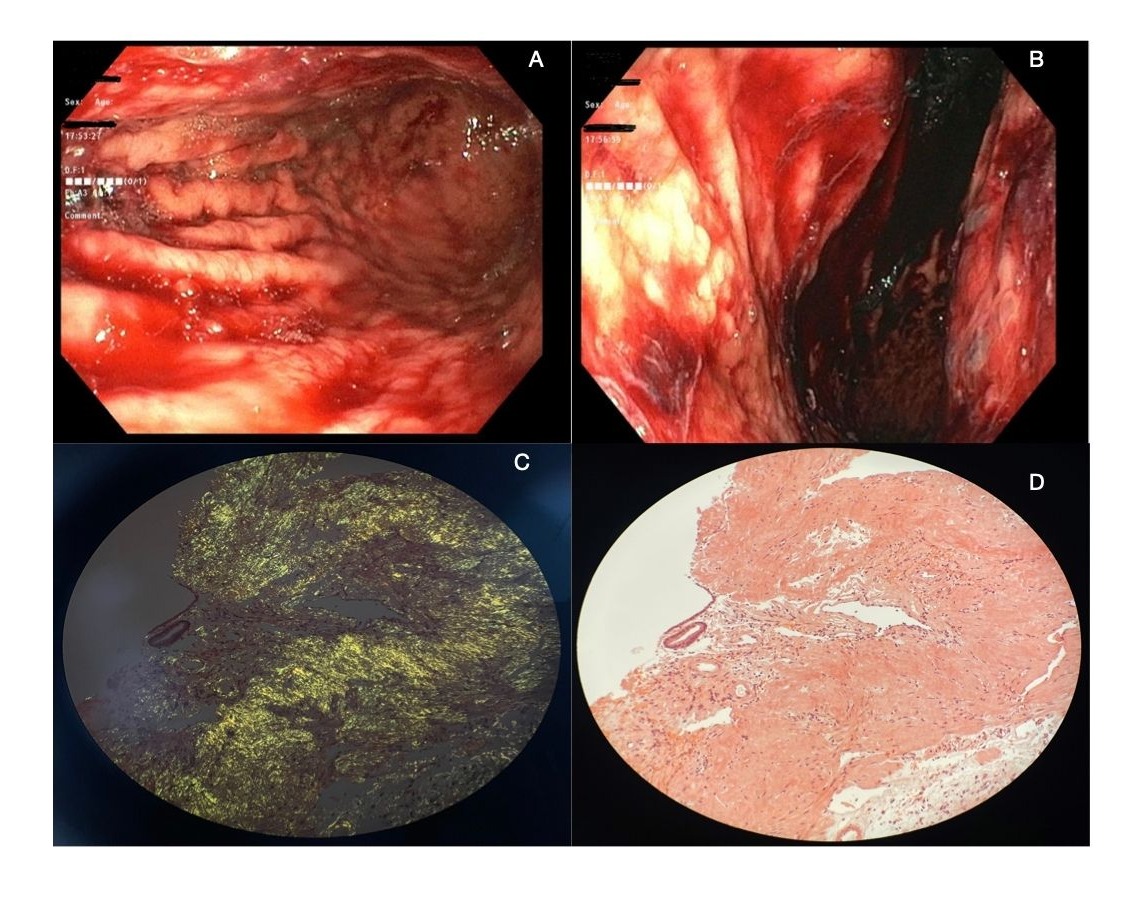
Case Description/Methods: A 59-year-old female presented to the emergency department with acute painless right eye subconjunctival hemorrhage, hematemesis and melena. Of note, patient had undergone a bone marrow and abdominal fat pad biopsy prior to her hospital presentation, which showed 10-15% plasma cells that stained negative for congo red. A computerized tomography angiography was ordered, which was concerning for a stomach mass. She underwent an upper endoscopy, which revealed clotted blood and diffuse nodular gastric mucosa with several areas that were oozing blood. The decision was made to start inpatient chemotherapy for her recent diagnosis of multiple myeloma, due to her ongoing GI bleeding. After her first chemotherapy session, her endoscopy pathology returned and showed abundant submucosal amorphous eosinophilic material suspicious for amyloid, which changed her course of treatment. Her chemotherapy regimen was adjusted, cardiac imaging studies were obtained and she was referred to a transplant center for stem cell transplant evaluation.
Discussion: AL amyloidosis is an acquired condition caused by a plasma cell dyscrasia with deposition of immunoglobulin light chains. Gastrointestinal symptoms are typically seen in systemic amyloid (79%) when compared to localized amyloid(21%). Due to complex clinical presentations, when amyloid is suspected, relevant imaging, laboratory testing and appropriate tissue collection is necessary for definitive diagnosis. Congo red stain used on tissue biopsies is the diagnostic gold standard, but tissue source does impact likelihood of positive results. Bone marrow sensitivity is 63% while kidney, liver or cardiac is 87-98%. Staging is performed at diagnosis to help determine prognosis and appropriate course of treatment. Treatment for AL amyloidosis is chemotherapy and stem cell transplantation.
Disclosures:
Andrea Schneider, DO1, Mehul Patel, DO2, Joseph Fares, MD3, Gavin Levinthal, MD3, Bassel Al-Lahham, MD1. P1644 - Gastric Amyloidosis: A Rare Case of Melena and Hematemesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HonorHealth, Phoenix, AZ; 2Honor Health Gastroenterology, Phoenix, AZ; 3HonorHealth, Scottsdale, AZ
Introduction: AL amyloidosis is a rare disorder caused by a clonal expansion of bone marrow plasma cells that secrete a monoclonal immunoglobulin light chain depositing as amyloid fibrils in tissues. 15% of these patients will have multiple myeloma. Although AL amyloid it is the most common type of amyloid seen, it is a rare condition, with an incidence of 9-14 cases per million and prevalence of 40.5 cases per million. Gastrointestinal bleeding due to amyloid deposition is infrequent. We describe a rare case of upper gastrointestinal bleeding that ultimately led to the diagnosis of GI amyloidosis in a patient who was recently diagnosed with multiple myeloma.
Case Description/Methods: A 59-year-old female presented to the emergency department with acute painless right eye subconjunctival hemorrhage, hematemesis and melena. Of note, patient had undergone a bone marrow and abdominal fat pad biopsy prior to her hospital presentation, which showed 10-15% plasma cells that stained negative for congo red. A computerized tomography angiography was ordered, which was concerning for a stomach mass. She underwent an upper endoscopy, which revealed clotted blood and diffuse nodular gastric mucosa with several areas that were oozing blood. The decision was made to start inpatient chemotherapy for her recent diagnosis of multiple myeloma, due to her ongoing GI bleeding. After her first chemotherapy session, her endoscopy pathology returned and showed abundant submucosal amorphous eosinophilic material suspicious for amyloid, which changed her course of treatment. Her chemotherapy regimen was adjusted, cardiac imaging studies were obtained and she was referred to a transplant center for stem cell transplant evaluation.
Discussion: AL amyloidosis is an acquired condition caused by a plasma cell dyscrasia with deposition of immunoglobulin light chains. Gastrointestinal symptoms are typically seen in systemic amyloid (79%) when compared to localized amyloid(21%). Due to complex clinical presentations, when amyloid is suspected, relevant imaging, laboratory testing and appropriate tissue collection is necessary for definitive diagnosis. Congo red stain used on tissue biopsies is the diagnostic gold standard, but tissue source does impact likelihood of positive results. Bone marrow sensitivity is 63% while kidney, liver or cardiac is 87-98%. Staging is performed at diagnosis to help determine prognosis and appropriate course of treatment. Treatment for AL amyloidosis is chemotherapy and stem cell transplantation.
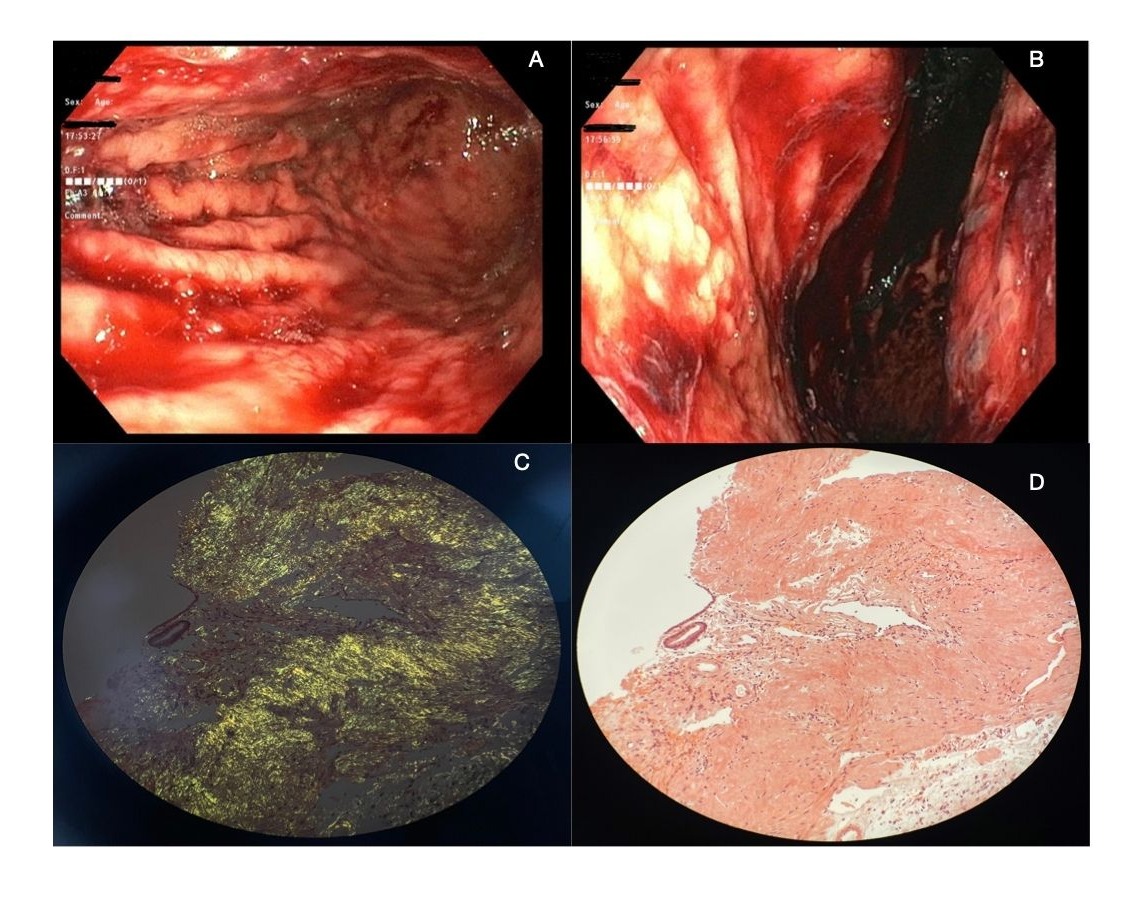
Figure: A Endoscopy showing red blood in the gastric body with nodular mucosa and thickened rugae.
B Endoscopy in retroflexed view showing red blood in the fundus and nodular mucosa
C Pathology showing apple-green birefringence with polarized light
D Pathology with positive Congo red stain
B Endoscopy in retroflexed view showing red blood in the fundus and nodular mucosa
C Pathology showing apple-green birefringence with polarized light
D Pathology with positive Congo red stain
Disclosures:
Andrea Schneider indicated no relevant financial relationships.
Mehul Patel indicated no relevant financial relationships.
Joseph Fares indicated no relevant financial relationships.
Gavin Levinthal indicated no relevant financial relationships.
Bassel Al-Lahham indicated no relevant financial relationships.
Andrea Schneider, DO1, Mehul Patel, DO2, Joseph Fares, MD3, Gavin Levinthal, MD3, Bassel Al-Lahham, MD1. P1644 - Gastric Amyloidosis: A Rare Case of Melena and Hematemesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
