Sunday Poster Session
Category: Stomach
P1650 - A Rare Case of Gastric Amyloidosis in a Patient With End-Stage Renal Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Pratiksha Moliya, MD
Jamaica Hospital Medical Center
Edison, NJ
Presenting Author(s)
Pratiksha Moliya, MD1, Hasan Al-Obaidi, MD2, Hima Varsha. Voruganti, MBBS, MD3, Utsav Moliya, MBBS4, Sophia Jagroop, MD5
1Jamaica Hospital Medical Center, Edison, NJ; 2Jamaica Hospital Medical Center, Briarwood, NY; 3North Alabama Medical Center, Florence, AL; 4College of Medical Sciences, Bharatpur, Narayani, Nepal; 5Jamaica Hospital Medical Center, Queens, NY
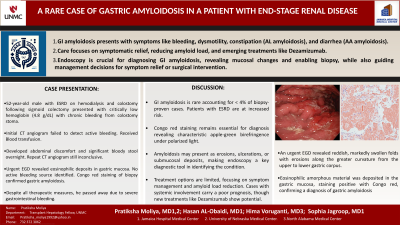
Introduction: Amyloidosis of the gastrointestinal (GI) tract is rare, accounting for less than 4% of biopsy-proven cases. Here, we report the first case of end-stage renal disease (ESRD)-related gastric amyloidosis, highlighting the challenges associated with its diagnosis and management.
Case Description/Methods: A 52-year-old male with multiple comorbidities, including a colostomy following sigmoid colectomy and ESRD on hemodialysis, was referred for critically low hemoglobin of 4.8 g/dL. Initially, his anemia was attributed to bleeding from decubitus ulcer, which surgery later determined was not a significant source of bleeding. He reported chronic bleeding from a colostomy stoma. His last endoscopy(EGD), performed 10 years ago, was unremarkable. CT angiogram failed to identify a definitive source of bleeding. He was hemodynamically stabilized. Overnight, he developed abdominal discomfort with significant bloody stool from stoma; Repeat CT angiogram did not show source of bleeding. Urgent EGD revealed gastric mucosa with eosinophilic amorphous material deposition, positive for Congo red stain consistent with amyloidosis. Regrettably, despite all therapeutic measures, he passed away due to severe gastrointestinal bleeding.
Discussion: Amyloidosis involves the deposition of extracellular protein forming ß-pleated sheets and affects the GI tract in both systemic and localized forms. Symptoms include anorexia, weight loss, GI bleeding, and chronic dysmotility. AL amyloidosis leads to intestinal symptoms like constipation or pseudo-obstruction due to thickened mucosal layers, while AA amyloidosis typically presents with diarrhea and malabsorption. Patients with ESRD-related amyloidosis, like the case discussed, often suffer from GI bleeding. Diagnosis is confirmed by biopsy with Congo red staining, which reveals characteristic apple-green birefringence under polarized light. The prognosis depends on the extent of involvement, the type of amyloid, and the amount of deposition. Advanced cases with liver involvement have poor outcomes. Systemic cases require treatment of the underlying condition, while localized forms may be treated with surgical excision. Management focuses on symptom alleviation and reducing amyloid load, with potential treatments including stem cell transplantation for AL amyloidosis. Treatment with the monoclonal antibody Dezamizumab is emerging, underscoring the necessity for a multidisciplinary approach to improve patient outcomes in GI amyloidosis.
Disclosures:
Pratiksha Moliya, MD1, Hasan Al-Obaidi, MD2, Hima Varsha. Voruganti, MBBS, MD3, Utsav Moliya, MBBS4, Sophia Jagroop, MD5. P1650 - A Rare Case of Gastric Amyloidosis in a Patient With End-Stage Renal Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jamaica Hospital Medical Center, Edison, NJ; 2Jamaica Hospital Medical Center, Briarwood, NY; 3North Alabama Medical Center, Florence, AL; 4College of Medical Sciences, Bharatpur, Narayani, Nepal; 5Jamaica Hospital Medical Center, Queens, NY
Introduction: Amyloidosis of the gastrointestinal (GI) tract is rare, accounting for less than 4% of biopsy-proven cases. Here, we report the first case of end-stage renal disease (ESRD)-related gastric amyloidosis, highlighting the challenges associated with its diagnosis and management.
Case Description/Methods: A 52-year-old male with multiple comorbidities, including a colostomy following sigmoid colectomy and ESRD on hemodialysis, was referred for critically low hemoglobin of 4.8 g/dL. Initially, his anemia was attributed to bleeding from decubitus ulcer, which surgery later determined was not a significant source of bleeding. He reported chronic bleeding from a colostomy stoma. His last endoscopy(EGD), performed 10 years ago, was unremarkable. CT angiogram failed to identify a definitive source of bleeding. He was hemodynamically stabilized. Overnight, he developed abdominal discomfort with significant bloody stool from stoma; Repeat CT angiogram did not show source of bleeding. Urgent EGD revealed gastric mucosa with eosinophilic amorphous material deposition, positive for Congo red stain consistent with amyloidosis. Regrettably, despite all therapeutic measures, he passed away due to severe gastrointestinal bleeding.
Discussion: Amyloidosis involves the deposition of extracellular protein forming ß-pleated sheets and affects the GI tract in both systemic and localized forms. Symptoms include anorexia, weight loss, GI bleeding, and chronic dysmotility. AL amyloidosis leads to intestinal symptoms like constipation or pseudo-obstruction due to thickened mucosal layers, while AA amyloidosis typically presents with diarrhea and malabsorption. Patients with ESRD-related amyloidosis, like the case discussed, often suffer from GI bleeding. Diagnosis is confirmed by biopsy with Congo red staining, which reveals characteristic apple-green birefringence under polarized light. The prognosis depends on the extent of involvement, the type of amyloid, and the amount of deposition. Advanced cases with liver involvement have poor outcomes. Systemic cases require treatment of the underlying condition, while localized forms may be treated with surgical excision. Management focuses on symptom alleviation and reducing amyloid load, with potential treatments including stem cell transplantation for AL amyloidosis. Treatment with the monoclonal antibody Dezamizumab is emerging, underscoring the necessity for a multidisciplinary approach to improve patient outcomes in GI amyloidosis.
Disclosures:
Pratiksha Moliya indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Hima Voruganti indicated no relevant financial relationships.
Utsav Moliya indicated no relevant financial relationships.
Sophia Jagroop indicated no relevant financial relationships.
Pratiksha Moliya, MD1, Hasan Al-Obaidi, MD2, Hima Varsha. Voruganti, MBBS, MD3, Utsav Moliya, MBBS4, Sophia Jagroop, MD5. P1650 - A Rare Case of Gastric Amyloidosis in a Patient With End-Stage Renal Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
