Sunday Poster Session
Category: Stomach
P1665 - A Challenging Case of Gastric Bezoar in a Patient on Tirzepatide
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KF
Kristen Fadel, MD
New York-Presbyterian Hospital/Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Kristen Fadel, MD1, Michelle Lee, MD1, Eliza Cricco-Lizza, MD2, Emily Smith, MD3, Laura Sahyoun, MD1, Ellen Scherl, MD1, Evan Grossman, MD1
1New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Gastric Bezoars are insoluble collections of ingested material, typically found in patients with an impaired grinding mechanism of the stomach or interdigestive migrating motor complex. Risk factors for development include prior gastric surgery, delayed gastric emptying, and anti-motility agents. Bezoars are initially managed conservatively with chemical dissolution, however if persistent may require endoscopic fragmentation.
Glucagon-like peptide-1 (GLP-1) agonists are increasingly being used to manage diabetes mellitus and obesity, and known side effects include nausea, vomiting, and delayed gastric emptying. We report a case of successful endoscopic management of a gastric bezoar in a patient with suspected gastroparesis secondary to tirzepatide.
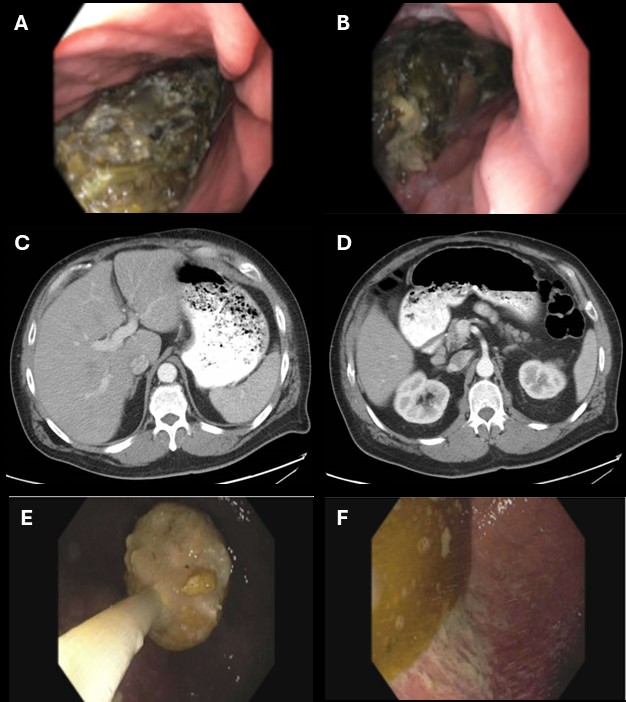
Case Description/Methods: A 46-year-old male with history of stricturing Crohn’s ileocolitis presented to his gastroenterologist with progressive nausea, vomiting, and abdominal pain. Outpatient esophagogastroduodenoscopy (EGD) revealed a new gastric phytobezoar extending to the cardia, thus the case was aborted due to high aspiration risk and the patient was admitted to the hospital. CT Abdomen revealed marked gastric distension without evidence of bowel obstruction or stricture. The patient had taken tirzepatide one week prior to presentation and required opiates inpatient for pain control. Chemical dissolution with cola was not tolerated, thus patient underwent repeat EGD under general anesthesia, which showed a persistent bezoar extending throughout the stomach. Despite two hours of management with a gastric lavage kit and net retrieval, a portion of the bezoar remained. The case was terminated to decrease risk of esophageal trauma with plan to repeat endoscopy as needed.
Given persistent symptoms, a third EGD was pursued. The remaining food bezoar was completely cleared with recurrent net retrieval and suctioning, with subsequent improvement in symptoms. The patient was counseled to avoid GLP-1 agonists and other anti-motility agents.
Discussion: Delayed gastric emptying is a well-known side effect of GLP-1 agonists and can cause intolerance of normal food substances in higher risk individuals. Additional caution should be taken in patients with autonomic dysfunction (i.e. diabetic neuropathy), complex anatomy (i.e. prior gastric surgery, stricturing Crohn’s disease), and those on other anti-motility agents (i.e. opioids, anticholinergics). In patients with gastric bezoar who fail conservative management, endoscopic removal should be considered.
Disclosures:
Kristen Fadel, MD1, Michelle Lee, MD1, Eliza Cricco-Lizza, MD2, Emily Smith, MD3, Laura Sahyoun, MD1, Ellen Scherl, MD1, Evan Grossman, MD1. P1665 - A Challenging Case of Gastric Bezoar in a Patient on Tirzepatide, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Gastric Bezoars are insoluble collections of ingested material, typically found in patients with an impaired grinding mechanism of the stomach or interdigestive migrating motor complex. Risk factors for development include prior gastric surgery, delayed gastric emptying, and anti-motility agents. Bezoars are initially managed conservatively with chemical dissolution, however if persistent may require endoscopic fragmentation.
Glucagon-like peptide-1 (GLP-1) agonists are increasingly being used to manage diabetes mellitus and obesity, and known side effects include nausea, vomiting, and delayed gastric emptying. We report a case of successful endoscopic management of a gastric bezoar in a patient with suspected gastroparesis secondary to tirzepatide.
Case Description/Methods: A 46-year-old male with history of stricturing Crohn’s ileocolitis presented to his gastroenterologist with progressive nausea, vomiting, and abdominal pain. Outpatient esophagogastroduodenoscopy (EGD) revealed a new gastric phytobezoar extending to the cardia, thus the case was aborted due to high aspiration risk and the patient was admitted to the hospital. CT Abdomen revealed marked gastric distension without evidence of bowel obstruction or stricture. The patient had taken tirzepatide one week prior to presentation and required opiates inpatient for pain control. Chemical dissolution with cola was not tolerated, thus patient underwent repeat EGD under general anesthesia, which showed a persistent bezoar extending throughout the stomach. Despite two hours of management with a gastric lavage kit and net retrieval, a portion of the bezoar remained. The case was terminated to decrease risk of esophageal trauma with plan to repeat endoscopy as needed.
Given persistent symptoms, a third EGD was pursued. The remaining food bezoar was completely cleared with recurrent net retrieval and suctioning, with subsequent improvement in symptoms. The patient was counseled to avoid GLP-1 agonists and other anti-motility agents.
Discussion: Delayed gastric emptying is a well-known side effect of GLP-1 agonists and can cause intolerance of normal food substances in higher risk individuals. Additional caution should be taken in patients with autonomic dysfunction (i.e. diabetic neuropathy), complex anatomy (i.e. prior gastric surgery, stricturing Crohn’s disease), and those on other anti-motility agents (i.e. opioids, anticholinergics). In patients with gastric bezoar who fail conservative management, endoscopic removal should be considered.
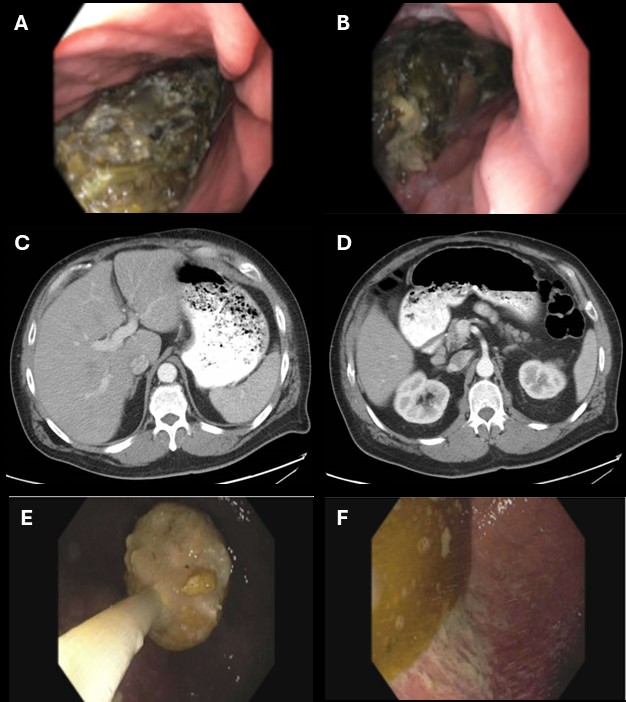
Figure: (A) Initial aborted EGD with bezoar in gastric body. (B) Initial aborted EGD with bezoar in gastric fundus. (C) CT Abdomen axial with gastric distension. (D) CT Abdomen axial demonstrating transition to normal caliber at 2nd portion of duodenum. (E) Final EGD, removing bezoar via net retrieval. (F) Final EGD, gastric fundus after bezoar completely cleared.
Disclosures:
Kristen Fadel indicated no relevant financial relationships.
Michelle Lee indicated no relevant financial relationships.
Eliza Cricco-Lizza indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Laura Sahyoun indicated no relevant financial relationships.
Ellen Scherl: Abbvie – Consultant, Speakers Bureau. BMS – Consultant, Speakers Bureau. Johnson and Johnson – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Evan Grossman indicated no relevant financial relationships.
Kristen Fadel, MD1, Michelle Lee, MD1, Eliza Cricco-Lizza, MD2, Emily Smith, MD3, Laura Sahyoun, MD1, Ellen Scherl, MD1, Evan Grossman, MD1. P1665 - A Challenging Case of Gastric Bezoar in a Patient on Tirzepatide, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
