Sunday Poster Session
Category: Stomach
P1688 - Shaken, Not Stirred: Unveiling Invasive Listeria Bacteremia From an Infected Milkshake
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SR
Sahalia Rashid, MD, PhD
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Sahalia Rashid, MD, PhD1, Anusha Majagi, MD2, Adam M. Qazi, MD3, Komal Mendiratta, MD2, Sharad Oli, MD2, Nicole Geissinger, MD2
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI; 3Detroit Medical Center/Wayne State University, Troy, MI
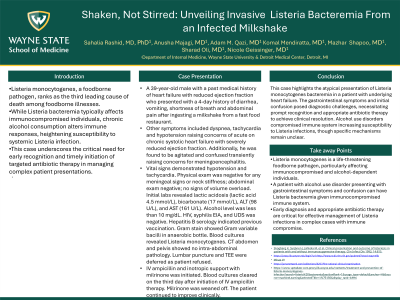
Introduction: Listeria monocytogenes, a foodborne pathogen, ranks as the third leading cause of death among foodborne illnesses. While Listeria bacteremia typically affects immunocompromised individuals, chronic alcohol consumption alters immune responses, heightening susceptibility to systemic Listeria infection. This case underscores the critical need for early recognition and timely initiation of targeted antibiotic therapy in managing complex patient presentations.
Case Description/Methods: A 39-year-old male with a past medical history of heart failure with reduced ejection fraction who presented with a 4-day history of diarrhea, vomiting, shortness of breath and abdominal pain after ingesting a milkshake from a fast food restaurant. Other symptoms included dyspnea with tachycardia and hypotension raising concerns of acute on chronic systolic heart failure with severely reduced ejection fraction. Additionally, he was found to be agitated and confused transiently raising concerns for meningoencephalitis. Vital signs demonstrated hypotension and tachycardia. Physical exam was negative for any meningeal signs or neck stiffness; abdominal exam negative; no signs of volume overload. Initial labs revealed lactic acidosis (lactic acid 4.5 mmol/L), bicarbonate deficiency (17 mmol/L), ALT (98 U/L), and AST (161 U/L). Alcohol level was less than 10 mg/dL. HIV, syphilis EIA, and urine drug screen were negative. Hepatitis B serology indicated previous vaccination. Gram stain demonstrated Gram variable bacilli in anaerobic bottle. Blood cultures demonstrated Listeria monocytogenes. CT abdomen and pelvis showed no intra-abdominal pathology. Lumbar puncture and TEE were deferred as patient refused. IV ampicillin and inotropic support with milrinone was initiated. Blood cultures cleared on the third day after initiation of IV ampicillin therapy. Milrinone was weaned off. The patient continued to improve clinically.
Discussion: This case highlights the atypical presentation of Listeria monocytogenes bacteremia in a patient with underlying heart failure. The gastrointestinal symptoms and initial confusion posed diagnostic challenges, necessitating prompt recognition and appropriate antibiotic therapy to achieve clinical resolution. Alcohol use disorders compromised immune system increasing susceptibility to Listeria infections, though specific mechanisms remain unclear.
Disclosures:
Sahalia Rashid, MD, PhD1, Anusha Majagi, MD2, Adam M. Qazi, MD3, Komal Mendiratta, MD2, Sharad Oli, MD2, Nicole Geissinger, MD2. P1688 - Shaken, Not Stirred: Unveiling Invasive <i>Listeria</i> Bacteremia From an Infected Milkshake, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI; 3Detroit Medical Center/Wayne State University, Troy, MI
Introduction: Listeria monocytogenes, a foodborne pathogen, ranks as the third leading cause of death among foodborne illnesses. While Listeria bacteremia typically affects immunocompromised individuals, chronic alcohol consumption alters immune responses, heightening susceptibility to systemic Listeria infection. This case underscores the critical need for early recognition and timely initiation of targeted antibiotic therapy in managing complex patient presentations.
Case Description/Methods: A 39-year-old male with a past medical history of heart failure with reduced ejection fraction who presented with a 4-day history of diarrhea, vomiting, shortness of breath and abdominal pain after ingesting a milkshake from a fast food restaurant. Other symptoms included dyspnea with tachycardia and hypotension raising concerns of acute on chronic systolic heart failure with severely reduced ejection fraction. Additionally, he was found to be agitated and confused transiently raising concerns for meningoencephalitis. Vital signs demonstrated hypotension and tachycardia. Physical exam was negative for any meningeal signs or neck stiffness; abdominal exam negative; no signs of volume overload. Initial labs revealed lactic acidosis (lactic acid 4.5 mmol/L), bicarbonate deficiency (17 mmol/L), ALT (98 U/L), and AST (161 U/L). Alcohol level was less than 10 mg/dL. HIV, syphilis EIA, and urine drug screen were negative. Hepatitis B serology indicated previous vaccination. Gram stain demonstrated Gram variable bacilli in anaerobic bottle. Blood cultures demonstrated Listeria monocytogenes. CT abdomen and pelvis showed no intra-abdominal pathology. Lumbar puncture and TEE were deferred as patient refused. IV ampicillin and inotropic support with milrinone was initiated. Blood cultures cleared on the third day after initiation of IV ampicillin therapy. Milrinone was weaned off. The patient continued to improve clinically.
Discussion: This case highlights the atypical presentation of Listeria monocytogenes bacteremia in a patient with underlying heart failure. The gastrointestinal symptoms and initial confusion posed diagnostic challenges, necessitating prompt recognition and appropriate antibiotic therapy to achieve clinical resolution. Alcohol use disorders compromised immune system increasing susceptibility to Listeria infections, though specific mechanisms remain unclear.
Disclosures:
Sahalia Rashid indicated no relevant financial relationships.
Anusha Majagi indicated no relevant financial relationships.
Adam Qazi indicated no relevant financial relationships.
Komal Mendiratta indicated no relevant financial relationships.
Sharad Oli indicated no relevant financial relationships.
Nicole Geissinger indicated no relevant financial relationships.
Sahalia Rashid, MD, PhD1, Anusha Majagi, MD2, Adam M. Qazi, MD3, Komal Mendiratta, MD2, Sharad Oli, MD2, Nicole Geissinger, MD2. P1688 - Shaken, Not Stirred: Unveiling Invasive <i>Listeria</i> Bacteremia From an Infected Milkshake, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
