Sunday Poster Session
Category: Stomach
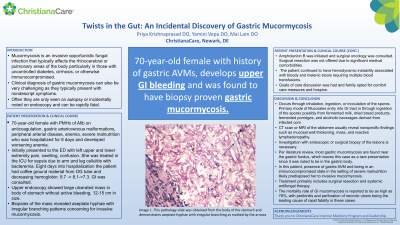
P1680 - Twists in the Gut: An Incidental Discovery of Gastric Mucormycosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Priya Krishnaprasad, DO
Christiana Care Health Services
Newark, DE
Presenting Author(s)
Priya Krishnaprasad, DO1, Yamini Vepa, DO2, Mai Lam, DO2
1Christiana Care Health Services, Newark, DE; 2Christiana Care Health System, Newark, DE
Introduction: Mucormycosis is an invasive opportunistic fungal infection that typically affects the rhinocerebral or pulmonary areas of the body particularly in those with uncontrolled diabetes, cirrhosis, or otherwise immunocompromised. Clinical diagnosis of gastric mucormycosis can also be very challenging as they typically present with nondescript symptoms. Often they are only seen on autopsy or incidentally noted on endoscopy and can be rapidly fatal.
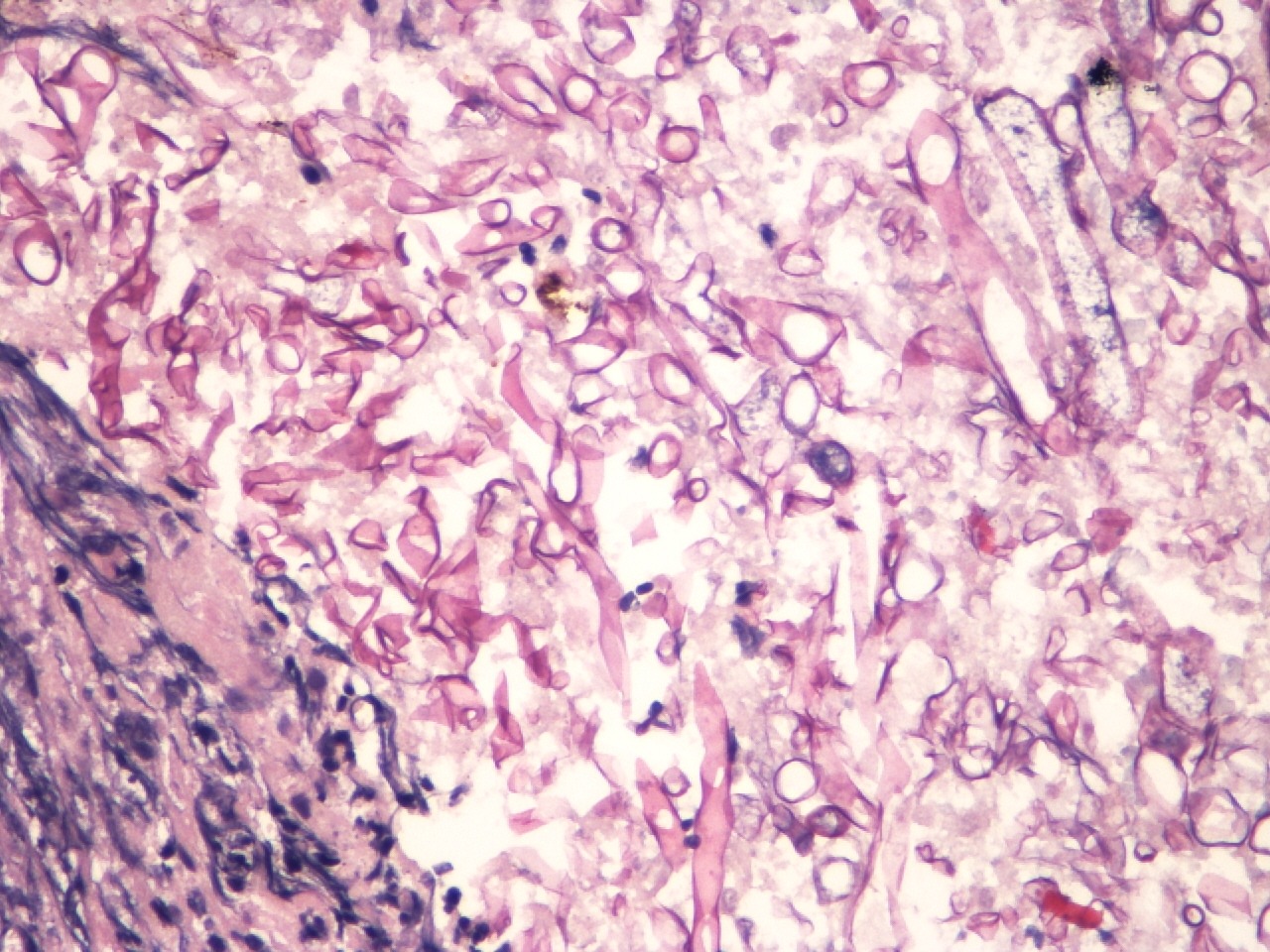
Case Description/Methods: A 70-year-old African American female with a history of atrial fibrillation on rivaroxaban, anemia, severe malnutrition, and gastric arteriovenous malformations (AVM) was admitted for sepsis secondary to left upper and lower extremity cellulitis with streptococcal bacteremia. Her course was complicated by upper GI bleeding, after which point an EGD was completed. The EGD incidentally revealed a 12-15 cm ulcerated mass in the gastric body, which was inconspicuous on a previous EGD four months prior. Biopsy showed aseptate hyphae with irregular branching patterns concerning for invasive mucormycosis. The patient was started on appropriate antimicrobial therapy, including amphotericin B, and was evaluated by surgical oncology. The surgical oncology team did not deem her to be a surgical candidate given her encephalopathy, severe malnutrition, and hemodynamic status. Ultimately, the patient and her family declined surgical intervention and pursued hospice.
Discussion: Gastric mucormycosis is quite rare and the primary mode of Mucorales entry into the GI tract is through ingestion of spores that may be found in items such as fermented milk, dried bread products, and alcoholic beverages derived from corn. CT scan or MRI imaging usually reveal nonspecific findings such as mucosal wall thickening, mass, and reactive lymphadenopathy. In fact, gastric mucormycosis is often found incidentally on endoscopy with biopsy or on autopsy. One hallmark of mucormycosis is angioinvasion and this patient’s history of AVM’s may have been a predisposing factor. Clinicians should be aware of the rapidly fatal nature of gastric mucormycosis with the mortality rate as high as 78%. Often peritonitis and perforation of necrotic ulcers are the leading causes of death in these cases.
Disclosures:
Priya Krishnaprasad, DO1, Yamini Vepa, DO2, Mai Lam, DO2. P1680 - Twists in the Gut: An Incidental Discovery of Gastric Mucormycosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Christiana Care Health Services, Newark, DE; 2Christiana Care Health System, Newark, DE
Introduction: Mucormycosis is an invasive opportunistic fungal infection that typically affects the rhinocerebral or pulmonary areas of the body particularly in those with uncontrolled diabetes, cirrhosis, or otherwise immunocompromised. Clinical diagnosis of gastric mucormycosis can also be very challenging as they typically present with nondescript symptoms. Often they are only seen on autopsy or incidentally noted on endoscopy and can be rapidly fatal.
Case Description/Methods: A 70-year-old African American female with a history of atrial fibrillation on rivaroxaban, anemia, severe malnutrition, and gastric arteriovenous malformations (AVM) was admitted for sepsis secondary to left upper and lower extremity cellulitis with streptococcal bacteremia. Her course was complicated by upper GI bleeding, after which point an EGD was completed. The EGD incidentally revealed a 12-15 cm ulcerated mass in the gastric body, which was inconspicuous on a previous EGD four months prior. Biopsy showed aseptate hyphae with irregular branching patterns concerning for invasive mucormycosis. The patient was started on appropriate antimicrobial therapy, including amphotericin B, and was evaluated by surgical oncology. The surgical oncology team did not deem her to be a surgical candidate given her encephalopathy, severe malnutrition, and hemodynamic status. Ultimately, the patient and her family declined surgical intervention and pursued hospice.
Discussion: Gastric mucormycosis is quite rare and the primary mode of Mucorales entry into the GI tract is through ingestion of spores that may be found in items such as fermented milk, dried bread products, and alcoholic beverages derived from corn. CT scan or MRI imaging usually reveal nonspecific findings such as mucosal wall thickening, mass, and reactive lymphadenopathy. In fact, gastric mucormycosis is often found incidentally on endoscopy with biopsy or on autopsy. One hallmark of mucormycosis is angioinvasion and this patient’s history of AVM’s may have been a predisposing factor. Clinicians should be aware of the rapidly fatal nature of gastric mucormycosis with the mortality rate as high as 78%. Often peritonitis and perforation of necrotic ulcers are the leading causes of death in these cases.
Figure: This is a biopsy taken from the gastric body showing numerous non-septated fungal hyphae representing invasive Mucormycosis.
Disclosures:
Priya Krishnaprasad indicated no relevant financial relationships.
Yamini Vepa indicated no relevant financial relationships.
Mai Lam indicated no relevant financial relationships.
Priya Krishnaprasad, DO1, Yamini Vepa, DO2, Mai Lam, DO2. P1680 - Twists in the Gut: An Incidental Discovery of Gastric Mucormycosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
