Sunday Poster Session
Category: Stomach
P1684 - Gastroduodenal Fistula Stemming From a Prior Ulcer Amid NSAID Use
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- GC
Gregory Capelli, DO
Aurora Healthcare
Milwaukee, WI
Presenting Author(s)
Gregory Capelli, DO, Aboud Affi, MD
Aurora Healthcare, Milwaukee, WI
Introduction: Acquired double pylorus is a rare condition in which a gastroduodenal fistula (GDF) adjacent to the antrum produces the appearance of a second pylorus. GDFs are typically associated with H. pylori or nonsteroidal anti-inflammatory (NSAID) use. Typically, patients are asymptomatic, and treatment focuses on eliminating underlying causes. Here, we present the case of a patient who developed a GDF, with an ulcer within the fistula tract, stemming from a prior ulcer amid NSAID use.
Case Description/Methods: A 74-year-old male with a history of joint pain and NSAID use presented for weight loss. On physical examination, he appeared well without distress, abdominal pain, or discomfort. Laboratory findings showed a hemoglobin (Hb) level of 10.7 g/dL and mean corpuscular volume (MCV) of 86.0 fl. Esophagogastroduodenoscopy (EGD) revealed a 12mm Forrest III ulcer in the antrum. Biopsies revealed mild chronic gastritis, without evidence of H. pylori infection. The patient was told to stop NSAIDs and was prescribed twice daily PPI. An EGD three months later displayed a 3mm remnant ulcer with granulation tissue and patchy erythema in the antrum, indicative of mucosal healing.
A year later, the patient presented with dizziness. He had been using supratherapeutic doses of NSAIDs for several months for knee pain. He denied nausea, vomiting, or abdominal pain, but reported melena. Laboratory findings showed a Hb of 4.3 g/dL and MCV of 76.0 fl. On examination, he appeared well without acute distress or abdominal pain. Repeat Hb following transfusion of three units of packed red blood cells was 8.3 g/dL. Repeat EGD identified a GDF at the previous ulcer site in the antrum. Additionally, a 3cm Forrest IIa ulcer was observed along the luminal wall of the fistula. Hemostasis was successfully achieved using epinephrine injection and bipolar electrocautery. Biopsies showed benign gastric mucosa without H. pylori infection. The patient experienced no post-procedural complications or recurrence of gastrointestinal hemorrhage. He was discharged with strict instructions to stop NSAIDs and was given twice daily PPI therapy.
Discussion: While the exact mechanism of fistula formation in cases of GDFs is unclear, we present a case in which the primary suspect for GDF formation is fistulation originating from a previous gastric antral ulcer, compounded by persistent NSAID usage. This case also underscores the possibility of concomitant gastric ulcers along the GDF tract in individuals continuing NSAID therapy.
Disclosures:
Gregory Capelli, DO, Aboud Affi, MD. P1684 - Gastroduodenal Fistula Stemming From a Prior Ulcer Amid NSAID Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Aurora Healthcare, Milwaukee, WI
Introduction: Acquired double pylorus is a rare condition in which a gastroduodenal fistula (GDF) adjacent to the antrum produces the appearance of a second pylorus. GDFs are typically associated with H. pylori or nonsteroidal anti-inflammatory (NSAID) use. Typically, patients are asymptomatic, and treatment focuses on eliminating underlying causes. Here, we present the case of a patient who developed a GDF, with an ulcer within the fistula tract, stemming from a prior ulcer amid NSAID use.
Case Description/Methods: A 74-year-old male with a history of joint pain and NSAID use presented for weight loss. On physical examination, he appeared well without distress, abdominal pain, or discomfort. Laboratory findings showed a hemoglobin (Hb) level of 10.7 g/dL and mean corpuscular volume (MCV) of 86.0 fl. Esophagogastroduodenoscopy (EGD) revealed a 12mm Forrest III ulcer in the antrum. Biopsies revealed mild chronic gastritis, without evidence of H. pylori infection. The patient was told to stop NSAIDs and was prescribed twice daily PPI. An EGD three months later displayed a 3mm remnant ulcer with granulation tissue and patchy erythema in the antrum, indicative of mucosal healing.
A year later, the patient presented with dizziness. He had been using supratherapeutic doses of NSAIDs for several months for knee pain. He denied nausea, vomiting, or abdominal pain, but reported melena. Laboratory findings showed a Hb of 4.3 g/dL and MCV of 76.0 fl. On examination, he appeared well without acute distress or abdominal pain. Repeat Hb following transfusion of three units of packed red blood cells was 8.3 g/dL. Repeat EGD identified a GDF at the previous ulcer site in the antrum. Additionally, a 3cm Forrest IIa ulcer was observed along the luminal wall of the fistula. Hemostasis was successfully achieved using epinephrine injection and bipolar electrocautery. Biopsies showed benign gastric mucosa without H. pylori infection. The patient experienced no post-procedural complications or recurrence of gastrointestinal hemorrhage. He was discharged with strict instructions to stop NSAIDs and was given twice daily PPI therapy.
Discussion: While the exact mechanism of fistula formation in cases of GDFs is unclear, we present a case in which the primary suspect for GDF formation is fistulation originating from a previous gastric antral ulcer, compounded by persistent NSAID usage. This case also underscores the possibility of concomitant gastric ulcers along the GDF tract in individuals continuing NSAID therapy.
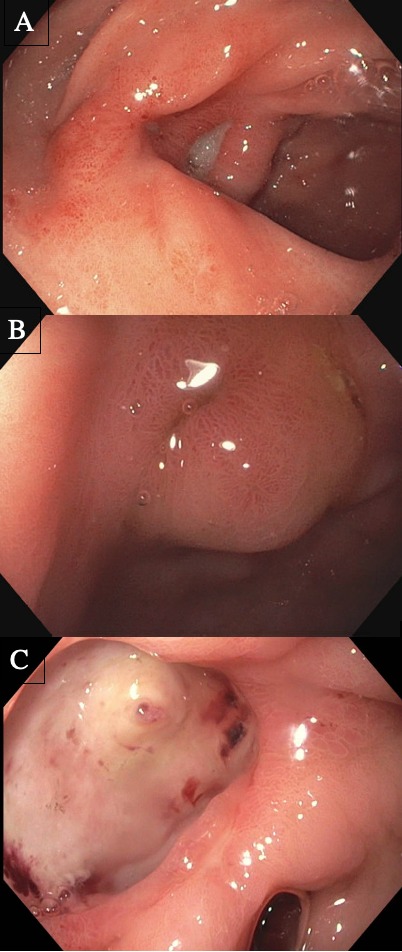
Figure: A. Initial EGD showing Forrest III ulcer in the antrum. B. EGD three months later showing interval reduction in ulcer size. C. EGD one year later showing a GDF situated at the site of the prior ulcer, with an additional Forrest IIa ulcer along the fistula tract.
Disclosures:
Gregory Capelli indicated no relevant financial relationships.
Aboud Affi indicated no relevant financial relationships.
Gregory Capelli, DO, Aboud Affi, MD. P1684 - Gastroduodenal Fistula Stemming From a Prior Ulcer Amid NSAID Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
