Sunday Poster Session
Category: Small Intestine
P1595 - Small Bowel Neuroendocrine Tumor Presenting With Chronic Diarrhea and Mesenteric Ischemia: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Shahem Abbarah, MD
MedStar Health
Baltimore, MD
Presenting Author(s)
Shahem Abbarah, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Bana Sabbagh, MD4, Abdellatif Ismail, MD5
1MedStar Health, Baltimore, MD; 2TriHealth, Doha, Ad Dawhah, Qatar; 3University of Toledo, Toledo, OH; 4TriHealth, Cincinnati, OH; 5University of Maryland Medical Center, Baltimore, MD
Introduction: Gastrointestinal (GI) neuroendocrine tumors (NETs) are a rare subset of neoplasms originating from neuroendocrine cells within the digestive tract. Despite their rarity, their incidence is increasing, necessitating a better understanding of their presentation and management.
Case Description/Methods: A 58-year-old Asian woman presented with a two-year history of chronic watery diarrhea, occasional diffuse crampy abdominal pain, and unintentional weight loss of 8 kg over the past year. She had multiple visits to the Emergency Department due to episodes of profuse, non-bloody diarrhea and dehydration.
The patient had a low body mass index of 18. Lab tests were unremarkable. During the upper endoscopy, a small subepithelial polypoid lesion with a central depression was found in the duodenal bulb. The colonoscopy showed congestion of the ileocecal valve, superficial ulcers, and edematous terminal ileum with a few aphthous ulcers. Biopsies were unremarkable. A CT enteroclysis revealed thickening in the terminal ileum, and an endoscopic ultrasound (EUS) identified a 16mm sub-epithelial lesion, which was diagnosed as a well-differentiated neuroendocrine tumor.
CT scan revealed mesenteric ischemia with pneumatosis intestinalis and portal venous gas. The pancreas showed air foci in the pancreatic head. After resuscitation, the patient underwent urgent diagnostic laparoscopy, which was converted to exploratory laparotomy. A patchy gangrenous segment involving the distal jejunum until the mid-ileum was resected. The proximal jejunum (150 cm from the duodenojejunal junction) and distal ileum (55 cm from the ileocecal valve) were preserved. Subsequent histopathological examination of the resected bowel segment confirmed acute transmural inflammation and necrosis consistent with ischemic bowel. Two days later, the patient underwent re-loop laparotomy, with the creation of a double-barrel stoma and abdominal closure.
The patient initially showed slight improvement but later experienced another drop in hemoglobin level and hypotension. Tests suggested possible vasculitis or vasospasm. a PET/CT scan revealed disease in the duodenum. The patient passed away two months after hospitalization due to recurrent infections.
Discussion: This case illuminates the diagnostic challenges associated with GI NETs, particularly in cases with nonspecific symptoms. It also underscores the importance of prompt recognition and management, as evidenced by the patient's progression to acute mesenteric ischemia.
Disclosures:
Shahem Abbarah, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Bana Sabbagh, MD4, Abdellatif Ismail, MD5. P1595 - Small Bowel Neuroendocrine Tumor Presenting With Chronic Diarrhea and Mesenteric Ischemia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Health, Baltimore, MD; 2TriHealth, Doha, Ad Dawhah, Qatar; 3University of Toledo, Toledo, OH; 4TriHealth, Cincinnati, OH; 5University of Maryland Medical Center, Baltimore, MD
Introduction: Gastrointestinal (GI) neuroendocrine tumors (NETs) are a rare subset of neoplasms originating from neuroendocrine cells within the digestive tract. Despite their rarity, their incidence is increasing, necessitating a better understanding of their presentation and management.
Case Description/Methods: A 58-year-old Asian woman presented with a two-year history of chronic watery diarrhea, occasional diffuse crampy abdominal pain, and unintentional weight loss of 8 kg over the past year. She had multiple visits to the Emergency Department due to episodes of profuse, non-bloody diarrhea and dehydration.
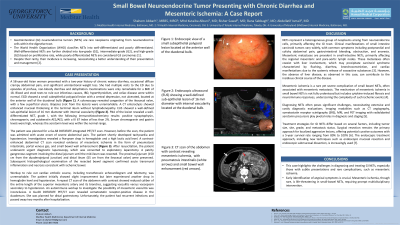
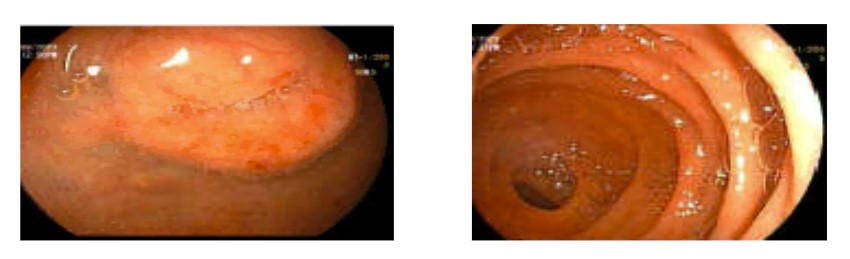
The patient had a low body mass index of 18. Lab tests were unremarkable. During the upper endoscopy, a small subepithelial polypoid lesion with a central depression was found in the duodenal bulb. The colonoscopy showed congestion of the ileocecal valve, superficial ulcers, and edematous terminal ileum with a few aphthous ulcers. Biopsies were unremarkable. A CT enteroclysis revealed thickening in the terminal ileum, and an endoscopic ultrasound (EUS) identified a 16mm sub-epithelial lesion, which was diagnosed as a well-differentiated neuroendocrine tumor.
CT scan revealed mesenteric ischemia with pneumatosis intestinalis and portal venous gas. The pancreas showed air foci in the pancreatic head. After resuscitation, the patient underwent urgent diagnostic laparoscopy, which was converted to exploratory laparotomy. A patchy gangrenous segment involving the distal jejunum until the mid-ileum was resected. The proximal jejunum (150 cm from the duodenojejunal junction) and distal ileum (55 cm from the ileocecal valve) were preserved. Subsequent histopathological examination of the resected bowel segment confirmed acute transmural inflammation and necrosis consistent with ischemic bowel. Two days later, the patient underwent re-loop laparotomy, with the creation of a double-barrel stoma and abdominal closure.
The patient initially showed slight improvement but later experienced another drop in hemoglobin level and hypotension. Tests suggested possible vasculitis or vasospasm. a PET/CT scan revealed disease in the duodenum. The patient passed away two months after hospitalization due to recurrent infections.
Discussion: This case illuminates the diagnostic challenges associated with GI NETs, particularly in cases with nonspecific symptoms. It also underscores the importance of prompt recognition and management, as evidenced by the patient's progression to acute mesenteric ischemia.
Figure: Small polypoid lesion with central depression, not ulcerated at the anterior wall of the duodenal bulb
Disclosures:
Shahem Abbarah indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Bana Sabbagh indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Shahem Abbarah, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Bana Sabbagh, MD4, Abdellatif Ismail, MD5. P1595 - Small Bowel Neuroendocrine Tumor Presenting With Chronic Diarrhea and Mesenteric Ischemia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
