Sunday Poster Session
Category: Stomach
P1599 - Response to Gastric Stimulation According to Gastroparesis vs Functional Dyspepsia Categorization
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Prateek Mathur, MD
University of Louisville
Louisville, KY
Presenting Author(s)
Prateek Mathur, MD1, Le Yu Naing, MD1, Syed Hassan Abbas, MD1, Lindsay McElmurray, PA-C1, Carmelita Moppins, APRN1, Michael Daniels, MS1, Abigail Stocker, MD2, Thomas Abell, MD2
1University of Louisville, Louisville, KY; 2University of Louisville School of Medicine, Louisville, KY
Introduction: Gastric electrical stimulation (GES) is a proven anti-emetic therapy for some patients, but its effect on other symptoms and if baseline gastric emptying affects symptoms (Sx) outcome of GES is unknown.
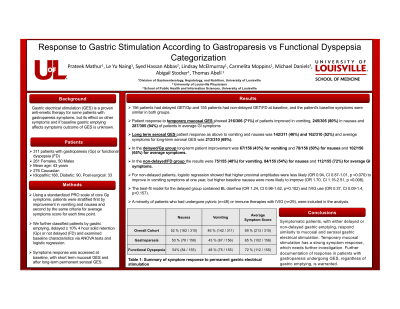
Methods: We examined symptom response of 311 patients with gastroparesis (Gp) or functional dyspepsia (FD) (261 f, 50 m, mean age 43 years, 276 Caucasian, 188 idiopathic, 90 diabetes, 33 post-surgical Gp) at baseline, with short term mucosal GES and after long-term permanent serosal GES. Using a standardized symptoms scale, patients were stratified by improvement in vomiting and nausea and average Sx score for each time point. We further classified patients by gastric emptying, delayed ≥ 10% 4 hr. solid retention (Gp) or not delayed (FD) and examined baseline characteristics via ANOVA tests and logistic regression.
Results: 56 patients had delayed GET/Gp, and 155 patients had non-delayed GET/FD at baseline. A minority had undergone pyloric (n=48) or immune therapies with IVIG (n=29), and were included in the analysis. Patient response to temporary mucosal GES showed 216/306 (71%) improved in vomiting, 245/305 (80%) in nausea and 287/305 (94%) in average GI Sx. Long term serosal GES patient response as above to vomiting and nausea was 142/311 (46%) & 162/310 (52%) and average symptoms for long-term serosal GES was 213/310 (69%). In the delayed/Gp group long-term improvement was 67/156 (43%) for vomiting and 78/156 (50%) for nausea & 102/156 (65%) for average Sx. In non-delayed/FD group, 75/155 (48%) for vomiting, 84/155 (54%) for nausea &112/155 (72%) for average. For non-delayed patients, logistic regression showed higher proximal amplitudes were less likely (OR 0.94, CI 0.87-1.01, p =0.070) to improve in vomiting symptoms; higher baseline nausea were more likely to improve (OR 1.70, CI 1.15-2.51, p =0.008). Best-fit model for delayed group included baseline diarrhea (OR 1.24, CI 0.96-1.62, p=0.102) & IVIG use (OR 0.37, CI 0.09-1.4, p=0.157).
Discussion: Symptomatic patients, with either delayed or non-delayed gastric emptying, respond similarly to mucosal and serosal gastric electrical stimulation. Temporary mucosal stimulation has a strong symptom response. Further documentation of response in patients undergoing GES, regardless of gastric emptying, is warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prateek Mathur, MD1, Le Yu Naing, MD1, Syed Hassan Abbas, MD1, Lindsay McElmurray, PA-C1, Carmelita Moppins, APRN1, Michael Daniels, MS1, Abigail Stocker, MD2, Thomas Abell, MD2. P1599 - Response to Gastric Stimulation According to Gastroparesis vs Functional Dyspepsia Categorization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Louisville, Louisville, KY; 2University of Louisville School of Medicine, Louisville, KY
Introduction: Gastric electrical stimulation (GES) is a proven anti-emetic therapy for some patients, but its effect on other symptoms and if baseline gastric emptying affects symptoms (Sx) outcome of GES is unknown.
Methods: We examined symptom response of 311 patients with gastroparesis (Gp) or functional dyspepsia (FD) (261 f, 50 m, mean age 43 years, 276 Caucasian, 188 idiopathic, 90 diabetes, 33 post-surgical Gp) at baseline, with short term mucosal GES and after long-term permanent serosal GES. Using a standardized symptoms scale, patients were stratified by improvement in vomiting and nausea and average Sx score for each time point. We further classified patients by gastric emptying, delayed ≥ 10% 4 hr. solid retention (Gp) or not delayed (FD) and examined baseline characteristics via ANOVA tests and logistic regression.
Results: 56 patients had delayed GET/Gp, and 155 patients had non-delayed GET/FD at baseline. A minority had undergone pyloric (n=48) or immune therapies with IVIG (n=29), and were included in the analysis. Patient response to temporary mucosal GES showed 216/306 (71%) improved in vomiting, 245/305 (80%) in nausea and 287/305 (94%) in average GI Sx. Long term serosal GES patient response as above to vomiting and nausea was 142/311 (46%) & 162/310 (52%) and average symptoms for long-term serosal GES was 213/310 (69%). In the delayed/Gp group long-term improvement was 67/156 (43%) for vomiting and 78/156 (50%) for nausea & 102/156 (65%) for average Sx. In non-delayed/FD group, 75/155 (48%) for vomiting, 84/155 (54%) for nausea &112/155 (72%) for average. For non-delayed patients, logistic regression showed higher proximal amplitudes were less likely (OR 0.94, CI 0.87-1.01, p =0.070) to improve in vomiting symptoms; higher baseline nausea were more likely to improve (OR 1.70, CI 1.15-2.51, p =0.008). Best-fit model for delayed group included baseline diarrhea (OR 1.24, CI 0.96-1.62, p=0.102) & IVIG use (OR 0.37, CI 0.09-1.4, p=0.157).
Discussion: Symptomatic patients, with either delayed or non-delayed gastric emptying, respond similarly to mucosal and serosal gastric electrical stimulation. Temporary mucosal stimulation has a strong symptom response. Further documentation of response in patients undergoing GES, regardless of gastric emptying, is warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prateek Mathur indicated no relevant financial relationships.
Le Yu Naing indicated no relevant financial relationships.
Syed Hassan Abbas indicated no relevant financial relationships.
Lindsay McElmurray indicated no relevant financial relationships.
Carmelita Moppins indicated no relevant financial relationships.
Michael Daniels indicated no relevant financial relationships.
Abigail Stocker indicated no relevant financial relationships.
Thomas Abell: ADEPT-GI – Intellectual Property/Patents, Owner/Ownership Interest. Enterra Medical – Consultant. Neurogastrx – Grant/Research Support. Nuvaira – Consultant. Processa – Grant/Research Support. UpToDate – Royalties. Vanda – Consultant, Grant/Research Support.
Prateek Mathur, MD1, Le Yu Naing, MD1, Syed Hassan Abbas, MD1, Lindsay McElmurray, PA-C1, Carmelita Moppins, APRN1, Michael Daniels, MS1, Abigail Stocker, MD2, Thomas Abell, MD2. P1599 - Response to Gastric Stimulation According to Gastroparesis vs Functional Dyspepsia Categorization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
