Sunday Poster Session
Category: Small Intestine
P1523 - Impact of Epidemiological and Tumor-related Factors on Survival Outcomes of Gastrointestinal Neuroendocrine Tumors: An Analysis of a Large Safety Net Hospital
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ramya Radhakrishnan, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Ramya Radhakrishnan, MD1, Grace Kim, MD1, Isa M. Jacoba, MD1, Qing Zhao, MD, PhD1, Haesook T. Kim, PhD2, Horst C. Weber, MD3
1Boston Medical Center, Boston, MA; 2Dana-Farber Cancer Institute, Boston, MA; 3Boston Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Neuroendocrine neoplasms (NEN) are a group of heterogeneous, rare tumors predominantly of the gastrointestinal (GI) tract. Despite their rise in incidence, NENs remain poorly understood overall. This study aims to examine the clinicopathological characteristics and prognosis of GI NENs in a racially and socioeconomically diverse population.
Methods: All patients at a large tertiary safety-net hospital with a pathology-proven GI NEN diagnosis within a 21-year period (2001-2022) were identified via the Clinical Data Warehouse. Liver NEN were considered metastatic in nature with unknown primary site. Patient and tumor characteristics, including age at diagnosis, race, sex, tumor site, tumor stage and size, were collected from medical charts. Overall survival (OS) was estimated by the Kaplan-Meier method and compared using log-rank test. Multivariable regression analysis for OS was performed using Cox model.
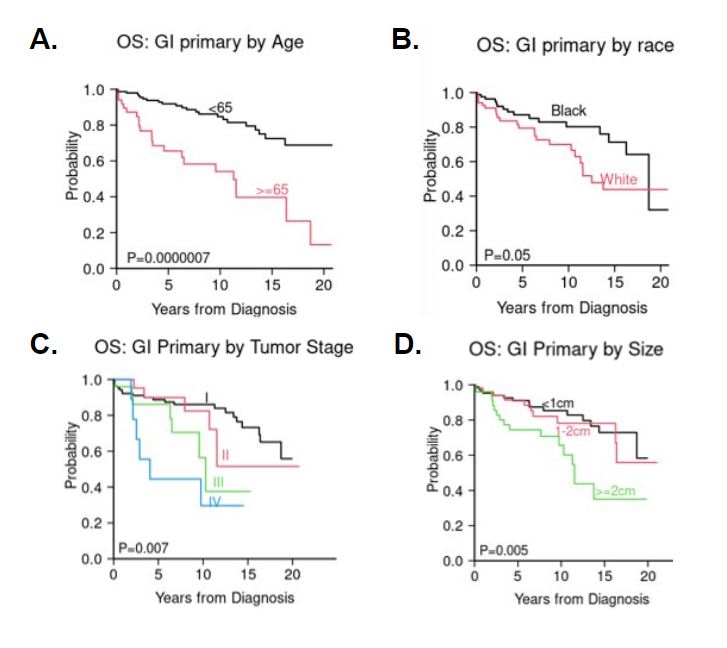
Results: A total of 222 patients (101 female [48.6%], 73 White [35.1%], 86 Black [41.3%], 10 Asian [4.8%]) received a diagnosis of GI NEN between 2001 and 2022, comprising of 208 GI primary tumors and 14 liver metastatic tumors (median age at diagnosis 55 and 68, respectively) (Table 1). Of all GI NENs, most localized to the rectum (N=57), followed by pancreas (N=47), small bowel (N=41), stomach (N=28), appendix (N=22), liver (N=14), and colon (N=13). The distribution of GI sites is significantly different between White and Black patients (p=0.007), with a higher incidence of colon, rectum, small bowel and stomach NENs in black patients. Age is significantly associated with overall survival (Hazard Ratio 4.37, p< 0.0001 for age >=65 compared to age< 65) (Fig 1A). Across all GI NEN subtypes, Black patients had similar OS to White patients (Fig 1B; 5-yr OS 87% vs 80%, p=0.05). GI NEN were diagnosed at stage TI in more than 50% of all patients and noted to have significantly better OS than higher T stage tumors (Fig 1C; P=0.01). Similarly, tumor size >2cm was associated with significantly shortened survival (Fig 1D; p=0.0025).
Discussion: This study demonstrated significant discordance in subtype distribution of GI NENs between white and black patients, a finding that is uniquely different from prior studies. It also shows similar OS in Black compared to White patients. The finding of distinct racial distributions amongst GI NEN subtypes and prognosis is a novel contribution towards improving diagnosis and treatment outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramya Radhakrishnan, MD1, Grace Kim, MD1, Isa M. Jacoba, MD1, Qing Zhao, MD, PhD1, Haesook T. Kim, PhD2, Horst C. Weber, MD3. P1523 - Impact of Epidemiological and Tumor-related Factors on Survival Outcomes of Gastrointestinal Neuroendocrine Tumors: An Analysis of a Large Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2Dana-Farber Cancer Institute, Boston, MA; 3Boston Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Neuroendocrine neoplasms (NEN) are a group of heterogeneous, rare tumors predominantly of the gastrointestinal (GI) tract. Despite their rise in incidence, NENs remain poorly understood overall. This study aims to examine the clinicopathological characteristics and prognosis of GI NENs in a racially and socioeconomically diverse population.
Methods: All patients at a large tertiary safety-net hospital with a pathology-proven GI NEN diagnosis within a 21-year period (2001-2022) were identified via the Clinical Data Warehouse. Liver NEN were considered metastatic in nature with unknown primary site. Patient and tumor characteristics, including age at diagnosis, race, sex, tumor site, tumor stage and size, were collected from medical charts. Overall survival (OS) was estimated by the Kaplan-Meier method and compared using log-rank test. Multivariable regression analysis for OS was performed using Cox model.
Results: A total of 222 patients (101 female [48.6%], 73 White [35.1%], 86 Black [41.3%], 10 Asian [4.8%]) received a diagnosis of GI NEN between 2001 and 2022, comprising of 208 GI primary tumors and 14 liver metastatic tumors (median age at diagnosis 55 and 68, respectively) (Table 1). Of all GI NENs, most localized to the rectum (N=57), followed by pancreas (N=47), small bowel (N=41), stomach (N=28), appendix (N=22), liver (N=14), and colon (N=13). The distribution of GI sites is significantly different between White and Black patients (p=0.007), with a higher incidence of colon, rectum, small bowel and stomach NENs in black patients. Age is significantly associated with overall survival (Hazard Ratio 4.37, p< 0.0001 for age >=65 compared to age< 65) (Fig 1A). Across all GI NEN subtypes, Black patients had similar OS to White patients (Fig 1B; 5-yr OS 87% vs 80%, p=0.05). GI NEN were diagnosed at stage TI in more than 50% of all patients and noted to have significantly better OS than higher T stage tumors (Fig 1C; P=0.01). Similarly, tumor size >2cm was associated with significantly shortened survival (Fig 1D; p=0.0025).
Discussion: This study demonstrated significant discordance in subtype distribution of GI NENs between white and black patients, a finding that is uniquely different from prior studies. It also shows similar OS in Black compared to White patients. The finding of distinct racial distributions amongst GI NEN subtypes and prognosis is a novel contribution towards improving diagnosis and treatment outcomes.
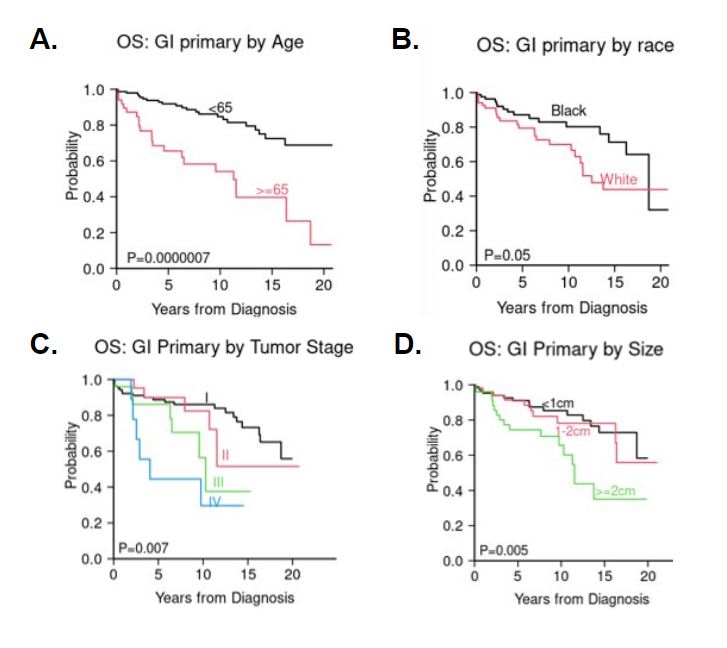
Figure: Overall survival of patients with primary gastrointestinal neuroendocrine neoplasms on the basis of age (A), race (B), tumor stage T I-IV (C) and size (D) estimated by Kaplan-Meier method and compared using log-rank test.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramya Radhakrishnan indicated no relevant financial relationships.
Grace Kim indicated no relevant financial relationships.
Isa Jacoba indicated no relevant financial relationships.
Qing Zhao indicated no relevant financial relationships.
Haesook Kim indicated no relevant financial relationships.
Horst Weber indicated no relevant financial relationships.
Ramya Radhakrishnan, MD1, Grace Kim, MD1, Isa M. Jacoba, MD1, Qing Zhao, MD, PhD1, Haesook T. Kim, PhD2, Horst C. Weber, MD3. P1523 - Impact of Epidemiological and Tumor-related Factors on Survival Outcomes of Gastrointestinal Neuroendocrine Tumors: An Analysis of a Large Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

