Sunday Poster Session
Category: Small Intestine
P1526 - Predictors of Bowel Dysfunction and Recovery in Hospitalized Cancer Patients: Treatment and Outcomes
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Sidra Naz, MD, MPH
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Sidra Naz, MD, MPH1, Irene J. Lee, MD2, Rohan Ahuja, MD3, Erini Gamal Nessim Kostandy, MD4, Jianliang Dai, PhD5, Mehnaz A. Shafi, MD1
1University of Texas MD Anderson Cancer Center, Houston, TX; 2Baylor College of Medicine, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX; 4The University of Texas MD Anderson Cancer Center, Houston, TX; 5MD Anderson Cancer Center, Houston, TX
Introduction: Bowel dysfunction is commonly observed in hospitalized cancer patients undergoing therapy. This condition is often exacerbated by opioid use, malnutrition, and prolonged bowel rest. Predictive causes of bowel dysfunction in cancer patients and effective treatments are not well known in this population. We aimed to identify the risk factors and assess the prevalence of opioid use and the use of peripherally acting Mu receptor antagonists for partial bowel obstruction in hospitalized cancer patients
Methods: We conducted a retrospective review of hospitalized cancer patients' charts with a radiological diagnosis of partial small or large bowel obstruction, or ileus, from January 2022 to April 2024 at a tertiary cancer hospital. Categorical variables were summarized by count and percentage and continuous variables were described by median and range (Min, Max) among outcome groups. The distributions of categorical and continuous variables among outcome groups were compared using Fisher’s exact test and the Kruskal-Wallis test, respectively. Predictors were analyzed by univariate ordinal logistic regression analysis to assess their individual effect on the outcome variable.
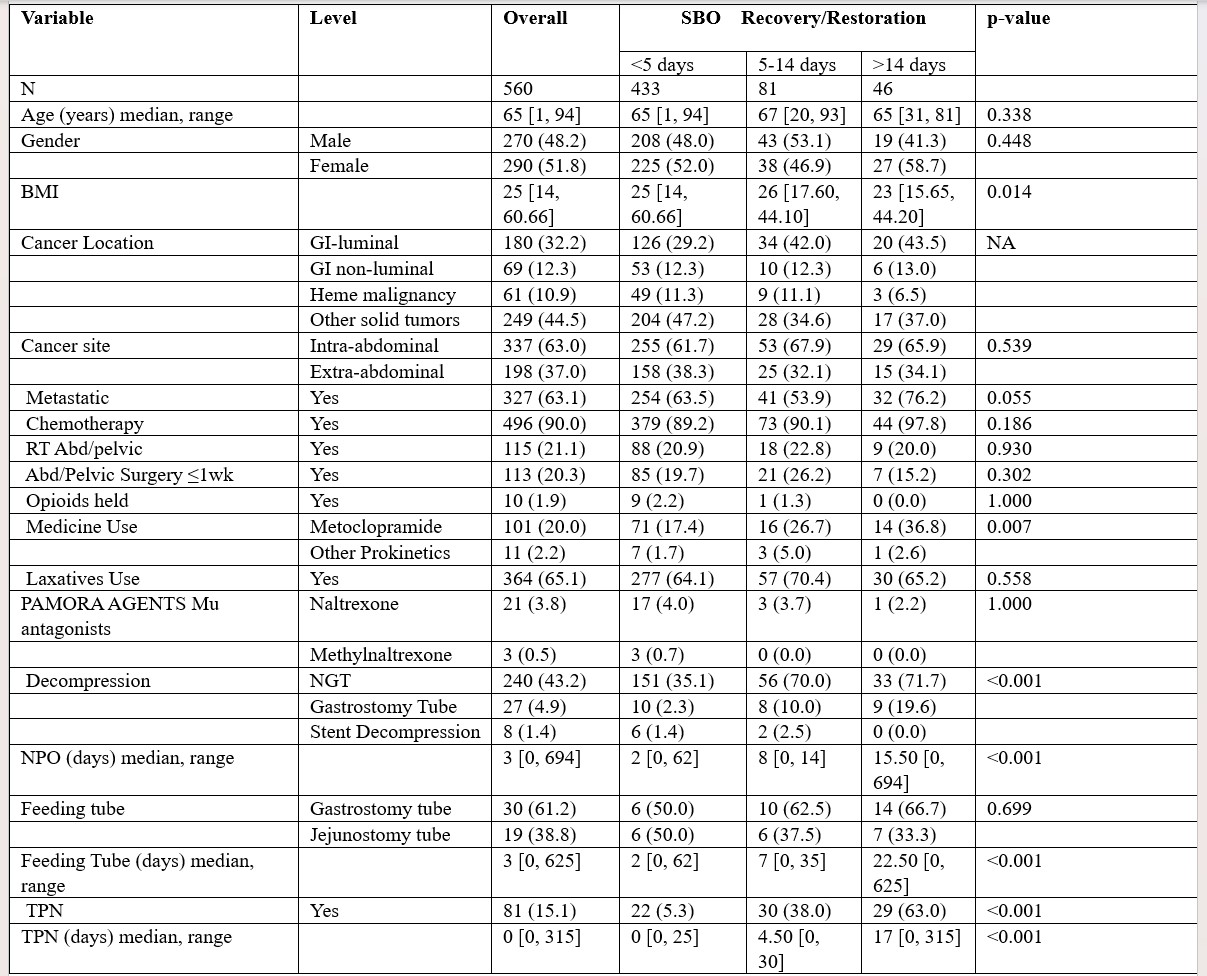
Results: 560 patients met the criteria had a median age of 65 years and BMI was 25, 51.8% were women, 68% were white, 10.8% black, 10.9% Hispanic. Cancer location was GI luminal in 180 (32.2%), GI non-luminal in 69 (12.3%). Opioid use was seen in 354 (63.7%) at the time of diagnosis. Despite 98% of patients having prior opioid use, less than 5% received a peripherally acting mu receptor antagonist. Metoclopramide use and NGT decompression were significantly associated with early bowel recovery (within 5 days). Prolonged bowel dysfunction was associated with prolonged use of TPN and a lower BMI. Bowel recovery/restoration was significantly associated with Decompression (Gastrostomy Tube OR (95%CI) =5.54 (2.06, 14.88), p< .001), NPO duration (OR (95%CI) =1.42 (1.27, 1.58), p< .001), and TPN duration in days (OR (95%CI) = 1.15 (1.08, 1.22), p< .001). GI lumen location adversely affected bowel recovery.
Discussion: Opioid use in hospitalized cancer patients with partial SBO or LBO, and ileus was 63.7% yet less than 5% received a PAMORA. Statistically significant predictors of early bowel recovery include the use of NGT decompression and metoclopramide. Prolonged use of TPN is associated with prolonged bowel dysfunction and a lower BMI. Increased use of prokinetics and PAMORA agents in this cohort may improve bowel recovery.
Disclosures:
Sidra Naz, MD, MPH1, Irene J. Lee, MD2, Rohan Ahuja, MD3, Erini Gamal Nessim Kostandy, MD4, Jianliang Dai, PhD5, Mehnaz A. Shafi, MD1. P1526 - Predictors of Bowel Dysfunction and Recovery in Hospitalized Cancer Patients: Treatment and Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas MD Anderson Cancer Center, Houston, TX; 2Baylor College of Medicine, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX; 4The University of Texas MD Anderson Cancer Center, Houston, TX; 5MD Anderson Cancer Center, Houston, TX
Introduction: Bowel dysfunction is commonly observed in hospitalized cancer patients undergoing therapy. This condition is often exacerbated by opioid use, malnutrition, and prolonged bowel rest. Predictive causes of bowel dysfunction in cancer patients and effective treatments are not well known in this population. We aimed to identify the risk factors and assess the prevalence of opioid use and the use of peripherally acting Mu receptor antagonists for partial bowel obstruction in hospitalized cancer patients
Methods: We conducted a retrospective review of hospitalized cancer patients' charts with a radiological diagnosis of partial small or large bowel obstruction, or ileus, from January 2022 to April 2024 at a tertiary cancer hospital. Categorical variables were summarized by count and percentage and continuous variables were described by median and range (Min, Max) among outcome groups. The distributions of categorical and continuous variables among outcome groups were compared using Fisher’s exact test and the Kruskal-Wallis test, respectively. Predictors were analyzed by univariate ordinal logistic regression analysis to assess their individual effect on the outcome variable.
Results: 560 patients met the criteria had a median age of 65 years and BMI was 25, 51.8% were women, 68% were white, 10.8% black, 10.9% Hispanic. Cancer location was GI luminal in 180 (32.2%), GI non-luminal in 69 (12.3%). Opioid use was seen in 354 (63.7%) at the time of diagnosis. Despite 98% of patients having prior opioid use, less than 5% received a peripherally acting mu receptor antagonist. Metoclopramide use and NGT decompression were significantly associated with early bowel recovery (within 5 days). Prolonged bowel dysfunction was associated with prolonged use of TPN and a lower BMI. Bowel recovery/restoration was significantly associated with Decompression (Gastrostomy Tube OR (95%CI) =5.54 (2.06, 14.88), p< .001), NPO duration (OR (95%CI) =1.42 (1.27, 1.58), p< .001), and TPN duration in days (OR (95%CI) = 1.15 (1.08, 1.22), p< .001). GI lumen location adversely affected bowel recovery.
Discussion: Opioid use in hospitalized cancer patients with partial SBO or LBO, and ileus was 63.7% yet less than 5% received a PAMORA. Statistically significant predictors of early bowel recovery include the use of NGT decompression and metoclopramide. Prolonged use of TPN is associated with prolonged bowel dysfunction and a lower BMI. Increased use of prokinetics and PAMORA agents in this cohort may improve bowel recovery.
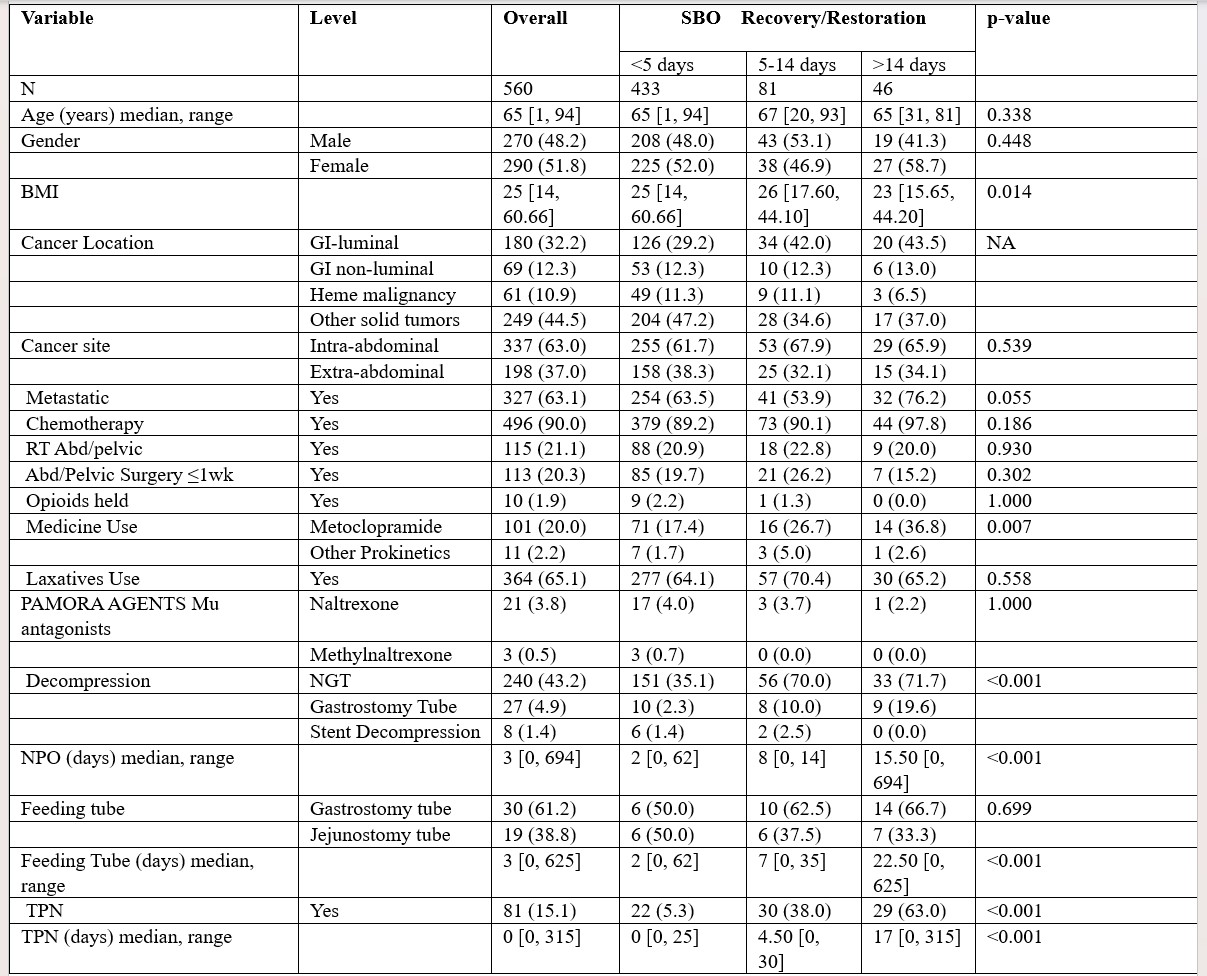
Figure: Table 1. Descriptive statistics of factors among SBO Recovery/Restoration Note: p-values were obtained from Fisher’s exact tests for categorical variables and the Kruskal-Wallis tests for continuous variables.
Disclosures:
Sidra Naz indicated no relevant financial relationships.
Irene Lee indicated no relevant financial relationships.
Rohan Ahuja indicated no relevant financial relationships.
Erini Gamal Nessim Kostandy indicated no relevant financial relationships.
Jianliang Dai indicated no relevant financial relationships.
Mehnaz Shafi indicated no relevant financial relationships.
Sidra Naz, MD, MPH1, Irene J. Lee, MD2, Rohan Ahuja, MD3, Erini Gamal Nessim Kostandy, MD4, Jianliang Dai, PhD5, Mehnaz A. Shafi, MD1. P1526 - Predictors of Bowel Dysfunction and Recovery in Hospitalized Cancer Patients: Treatment and Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
