Sunday Poster Session
Category: Small Intestine
P1529 - Hereditary Alpha-Tryptasemia Can Coexist With Celiac Disease and Be Associated With Non-Responsive Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Amelie Therrien, MD, MS
Beth Israel Deaconess Medical Center, Harvard Medical School
Boston, MA
Presenting Author(s)
Amelie Therrien, MD, MS1, Srihitha Akula, BS1, Michelle Galeas-Pena, MD, PhD2, Emma Frank, BS1, Lily Gillette, BS3, Jocelyn Silvester, MD, PhD3, Daniel Leffler, MD, MS1, Olga Pozdnyakova, MD, PhD4, Jonathan Lyons, MD5, Sarah C. Glover, DO6
1Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 2Tulane University, New Orleans, LA; 3Boston Children's Hospital, Boston, MA; 4University of Pennsylvania, Philadelphia, PA; 5University of California San Diego, La Jolla, CA; 6Tulane University School of Medicine, New Orleans, LA
Introduction: Hereditary alpha-tryptasemia (HαT) is characterized by an increased copy number of TPSAB1 which encodes α-tryptase, resulting in elevated basal serum tryptase. It is found in 5-7% of Western populations. Many individuals with HαT report irritable bowel syndrome-like and reflux symptoms. Our aim is to assess the prevalence of HαT in celiac disease (CeD) and determine whether this common genetic trait modifies symptoms or disease course.
Methods: Subjects with CeD or non-celiac gluten sensitivity (NCGS) were prospectively enrolled at a Celiac Center, either at the time of diagnosis (Dx), evaluation for non-responsive celiac disease (NRCD; symptoms despite being on a gluten-free diet) or while in clinical remission. Tryptase levels were obtained (Quest Diagnostics), and tryptase genotyping was performed on gDNA using ddPCR. Archived duodenal and stomach biopsies were stained with c-KIT (Dako, polyclonal dilution 1:1000), and mast cells (MC) counts were averaged per 5 hpf.
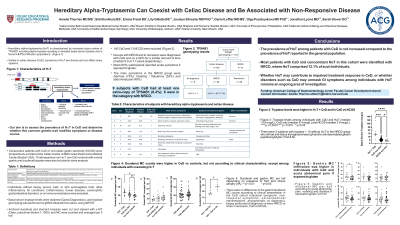
Results: TPSAB1 data was available for 142 eligible subjects; 12 NCGS and 130 CeD, which included newly Dx patients n=8, NRCD n=65, and individuals in remission n=57. HαT was found in 10 subjects with CeD (7.7%). All subjects with HαT had GI symptoms; 8 were in the NRCD subgroup (12.3%), 1 was in the remission group (1.75%), but had a history of chronic diarrhea controlled with diet that was considered as IBS-D, and 1 was a newly Dx CeD (12.5%). Excluding HαT cases, basal tryptase levels were higher among CeD vs NCGS (median 5.3 vs 3.6 mcg/L p< 0.01). Fifty patients, including 6 cases with HαT+CeD had available gastric and duodenal biopsies stained with c-kit. There were higher duodenal MC counts with CeD vs controls, but no difference within CeD group according to HαT (median HαT + CeD 27.3/hpf, non-HαT CeD 24.9 /hpf, controls 18.4/hpf). Gastric MC count was higher in subjects with acute abdominal pain if exposed to gluten (median 18.9/hpf vs 10.9/hpf p< 0.03). There was otherwise no difference in gastroduodenal MC count based on villous atrophy or clinical presentation.
Discussion: The prevalence of HαT in CeD is similar to the one reported in the general population. Remarkably, all patients with CeD and concomitant HαT in this cohort had GI symptoms and most were identified during an encounter for NRCD. Whether HαT may contribute to impaired treatment response in CeD, or whether disorders such as CeD may unmask GI symptoms among individuals with HαT remains an ongoing area of investigation.
Disclosures:
Amelie Therrien, MD, MS1, Srihitha Akula, BS1, Michelle Galeas-Pena, MD, PhD2, Emma Frank, BS1, Lily Gillette, BS3, Jocelyn Silvester, MD, PhD3, Daniel Leffler, MD, MS1, Olga Pozdnyakova, MD, PhD4, Jonathan Lyons, MD5, Sarah C. Glover, DO6. P1529 - Hereditary Alpha-Tryptasemia Can Coexist With Celiac Disease and Be Associated With Non-Responsive Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 2Tulane University, New Orleans, LA; 3Boston Children's Hospital, Boston, MA; 4University of Pennsylvania, Philadelphia, PA; 5University of California San Diego, La Jolla, CA; 6Tulane University School of Medicine, New Orleans, LA
Introduction: Hereditary alpha-tryptasemia (HαT) is characterized by an increased copy number of TPSAB1 which encodes α-tryptase, resulting in elevated basal serum tryptase. It is found in 5-7% of Western populations. Many individuals with HαT report irritable bowel syndrome-like and reflux symptoms. Our aim is to assess the prevalence of HαT in celiac disease (CeD) and determine whether this common genetic trait modifies symptoms or disease course.
Methods: Subjects with CeD or non-celiac gluten sensitivity (NCGS) were prospectively enrolled at a Celiac Center, either at the time of diagnosis (Dx), evaluation for non-responsive celiac disease (NRCD; symptoms despite being on a gluten-free diet) or while in clinical remission. Tryptase levels were obtained (Quest Diagnostics), and tryptase genotyping was performed on gDNA using ddPCR. Archived duodenal and stomach biopsies were stained with c-KIT (Dako, polyclonal dilution 1:1000), and mast cells (MC) counts were averaged per 5 hpf.
Results: TPSAB1 data was available for 142 eligible subjects; 12 NCGS and 130 CeD, which included newly Dx patients n=8, NRCD n=65, and individuals in remission n=57. HαT was found in 10 subjects with CeD (7.7%). All subjects with HαT had GI symptoms; 8 were in the NRCD subgroup (12.3%), 1 was in the remission group (1.75%), but had a history of chronic diarrhea controlled with diet that was considered as IBS-D, and 1 was a newly Dx CeD (12.5%). Excluding HαT cases, basal tryptase levels were higher among CeD vs NCGS (median 5.3 vs 3.6 mcg/L p< 0.01). Fifty patients, including 6 cases with HαT+CeD had available gastric and duodenal biopsies stained with c-kit. There were higher duodenal MC counts with CeD vs controls, but no difference within CeD group according to HαT (median HαT + CeD 27.3/hpf, non-HαT CeD 24.9 /hpf, controls 18.4/hpf). Gastric MC count was higher in subjects with acute abdominal pain if exposed to gluten (median 18.9/hpf vs 10.9/hpf p< 0.03). There was otherwise no difference in gastroduodenal MC count based on villous atrophy or clinical presentation.
Discussion: The prevalence of HαT in CeD is similar to the one reported in the general population. Remarkably, all patients with CeD and concomitant HαT in this cohort had GI symptoms and most were identified during an encounter for NRCD. Whether HαT may contribute to impaired treatment response in CeD, or whether disorders such as CeD may unmask GI symptoms among individuals with HαT remains an ongoing area of investigation.
Disclosures:
Amelie Therrien indicated no relevant financial relationships.
Srihitha Akula indicated no relevant financial relationships.
Michelle Galeas-Pena indicated no relevant financial relationships.
Emma Frank indicated no relevant financial relationships.
Lily Gillette indicated no relevant financial relationships.
Jocelyn Silvester indicated no relevant financial relationships.
Daniel Leffler: Takeda Pharmaceuticals – Employee.
Olga Pozdnyakova indicated no relevant financial relationships.
Jonathan Lyons: Blueprint Medicines – Consultant. Human Immunology Biosciences, Inc. – Consultant. Visterra, Inc. – Consultant.
Sarah C. Glover indicated no relevant financial relationships.
Amelie Therrien, MD, MS1, Srihitha Akula, BS1, Michelle Galeas-Pena, MD, PhD2, Emma Frank, BS1, Lily Gillette, BS3, Jocelyn Silvester, MD, PhD3, Daniel Leffler, MD, MS1, Olga Pozdnyakova, MD, PhD4, Jonathan Lyons, MD5, Sarah C. Glover, DO6. P1529 - Hereditary Alpha-Tryptasemia Can Coexist With Celiac Disease and Be Associated With Non-Responsive Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

