Sunday Poster Session
Category: Liver
P1428 - Gallbladder, Liver, or Infection?: A Case of an Atypical Autoimmune Hepatitis Presentation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Elizabeth Li, MD
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Elizabeth Li, MD1, Manasa Vallabhaneni, MD1, Joanne Lin, DO2, Kimberly Forde, MD, PhD1, Carolyn Hogan, MD1
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Autoimmune hepatitis (AIH) is a chronic liver disease that often manifests with nonspecific symptoms such as fatigue, abdominal pain, nausea, and jaundice. Overlap syndromes may include findings of AIH with another pathology, such as primary sclerosing cholangitis (PSC). At times, it is important to have a suspicion for AIH and overlap syndrome even if patients’ clinical presentations appear to be cholestatic in origin.
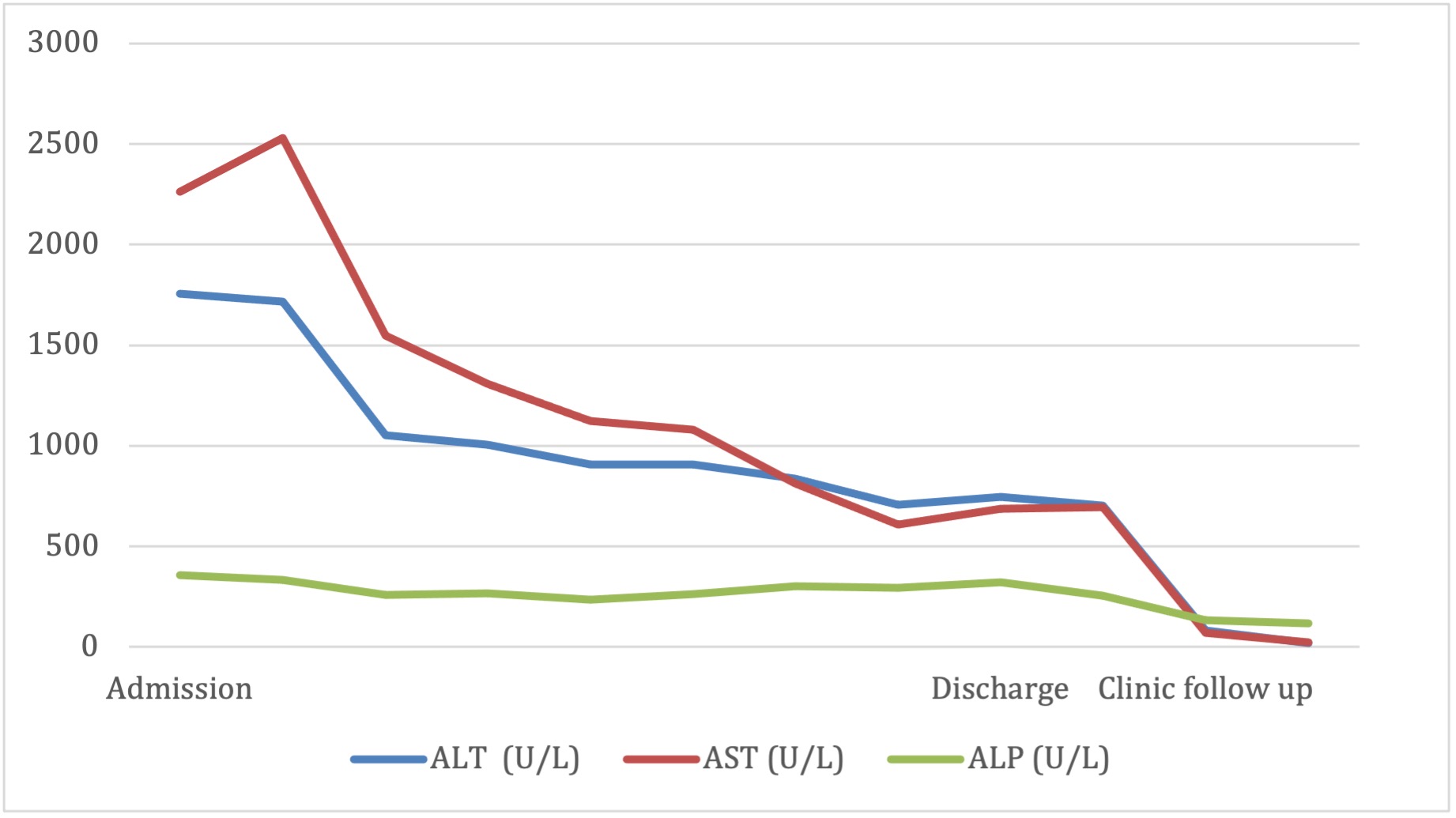
Case Description/Methods: A 46-year-old female with a history of class 2 obesity, hypertension, pre-diabetes, hyperlipidemia, peptic ulcer disease, hysterectomy and tubal ligation, and cervical spine fusion presented to the hospital with six days of RUQ and epigastric abdominal pain. Initial laboratory results showed a mixed pattern of liver injury, including elevated ALT 1757 U/L, AST 2262 U/L, ALP 355 U/L, INR 1.5, total bilirubin 4-5 mg/dL, and direct bilirubin 3 mg/dL. Patient denied a personal and family history of liver disease. She denied recent alcohol, tobacco, and drug use.
Given initial concern for choledocholithiasis, an MRCP and EUS were pursued. Both were negative for choledocholithiasis. Serological workup revealed a positive ANA 1:640, ASMA 1:320, and an elevated IgG of 1964. CMV and VZV IgM and IgG were also positive, but a CMV DNA viral load was negative. Infectious Diseases did not believe infection was the cause of her acute liver injury. A liver biopsy was obtained, which revealed portal inflammation with plasma cells suggestive of AIH with overlap of “onion-skinning” fibrosis around bile ducts suspicious for PSC. Moderate to severe cholestatic injury and fibrosis stage 2-3 of 4 were also noted. She was started on budesonide and at her clinic follow-up visit 2 weeks later, her labs slightly improved except for an AST which remained elevated. Budesonide was continued and ursodiol was added. Azathioprine was started after her labs further improved. Her hepatic function panel has normalized now leading to plans for a steroid taper.
Discussion: This case features a diagnosis of AIH with PSC overlap syndrome but with a nonspecific presentation that leads to suspicion of choledocholithiasis. It is well known that the clinical presentation of AIH can be nonspecific and highly variable. Acute AIH can mimic other conditions such as acute viral hepatitis and rarely choledocholithiasis. Our case highlights the importance of having a high clinical suspicion of AIH to avoid unnecessary interventions and facilitate initiation of proper treatment in a timely manner.
Disclosures:
Elizabeth Li, MD1, Manasa Vallabhaneni, MD1, Joanne Lin, DO2, Kimberly Forde, MD, PhD1, Carolyn Hogan, MD1. P1428 - Gallbladder, Liver, or Infection?: A Case of an Atypical Autoimmune Hepatitis Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Autoimmune hepatitis (AIH) is a chronic liver disease that often manifests with nonspecific symptoms such as fatigue, abdominal pain, nausea, and jaundice. Overlap syndromes may include findings of AIH with another pathology, such as primary sclerosing cholangitis (PSC). At times, it is important to have a suspicion for AIH and overlap syndrome even if patients’ clinical presentations appear to be cholestatic in origin.
Case Description/Methods: A 46-year-old female with a history of class 2 obesity, hypertension, pre-diabetes, hyperlipidemia, peptic ulcer disease, hysterectomy and tubal ligation, and cervical spine fusion presented to the hospital with six days of RUQ and epigastric abdominal pain. Initial laboratory results showed a mixed pattern of liver injury, including elevated ALT 1757 U/L, AST 2262 U/L, ALP 355 U/L, INR 1.5, total bilirubin 4-5 mg/dL, and direct bilirubin 3 mg/dL. Patient denied a personal and family history of liver disease. She denied recent alcohol, tobacco, and drug use.
Given initial concern for choledocholithiasis, an MRCP and EUS were pursued. Both were negative for choledocholithiasis. Serological workup revealed a positive ANA 1:640, ASMA 1:320, and an elevated IgG of 1964. CMV and VZV IgM and IgG were also positive, but a CMV DNA viral load was negative. Infectious Diseases did not believe infection was the cause of her acute liver injury. A liver biopsy was obtained, which revealed portal inflammation with plasma cells suggestive of AIH with overlap of “onion-skinning” fibrosis around bile ducts suspicious for PSC. Moderate to severe cholestatic injury and fibrosis stage 2-3 of 4 were also noted. She was started on budesonide and at her clinic follow-up visit 2 weeks later, her labs slightly improved except for an AST which remained elevated. Budesonide was continued and ursodiol was added. Azathioprine was started after her labs further improved. Her hepatic function panel has normalized now leading to plans for a steroid taper.
Discussion: This case features a diagnosis of AIH with PSC overlap syndrome but with a nonspecific presentation that leads to suspicion of choledocholithiasis. It is well known that the clinical presentation of AIH can be nonspecific and highly variable. Acute AIH can mimic other conditions such as acute viral hepatitis and rarely choledocholithiasis. Our case highlights the importance of having a high clinical suspicion of AIH to avoid unnecessary interventions and facilitate initiation of proper treatment in a timely manner.
Figure: LFT Trend
Disclosures:
Elizabeth Li indicated no relevant financial relationships.
Manasa Vallabhaneni indicated no relevant financial relationships.
Joanne Lin indicated no relevant financial relationships.
Kimberly Forde indicated no relevant financial relationships.
Carolyn Hogan indicated no relevant financial relationships.
Elizabeth Li, MD1, Manasa Vallabhaneni, MD1, Joanne Lin, DO2, Kimberly Forde, MD, PhD1, Carolyn Hogan, MD1. P1428 - Gallbladder, Liver, or Infection?: A Case of an Atypical Autoimmune Hepatitis Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

