Sunday Poster Session
Category: Liver
P1432 - Hepatocellular Adenoma Presenting With Concomitant Rupture and Hepatocellular Carcinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Emuejevuoke Umukoro, DO
Scripps Mercy Hospital
San Ysidro, CA
Presenting Author(s)
Emuejevuoke Umukoro, DO1, Kevin Pak, MD2, Julio A. Gutierrez, MD3
1Scripps Mercy Hospital, San Ysidro, CA; 2Naval Medical Center San Diego, San Diego, CA; 3Scripps Clinic, San Diego, CA
Introduction: Hepatocellular adenomas (HCAs) are rare, benign neoplasms from monoclonal proliferation of mature hepatocytes. HCAs mainly occurs in women using oral contraceptive pills (OCPs), but the true population incidence is unknown. It occurs less in men; but the incidence has increased since the 1980s. Though often benign, HCAs can have malignant transformation into hepatocellular carcinoma (HCC). We present a case of a male patient who was found to have a HCA with hepatocellular carcinoma (HCC).
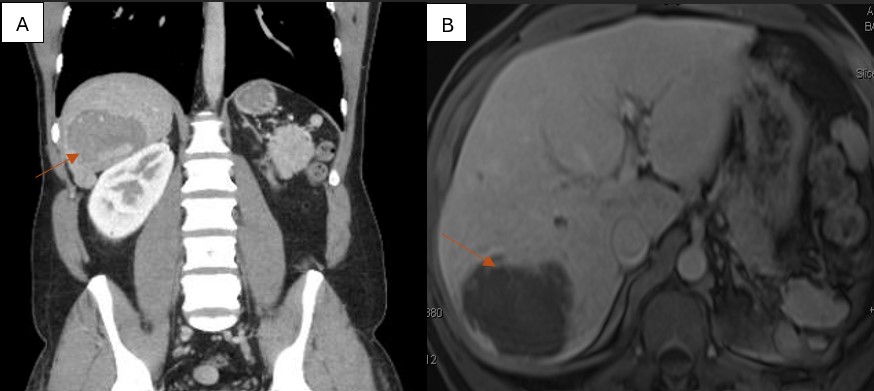
Case Description/Methods: A 44-year-old-male with past medical history of trauma status post left nephrectomy and splenectomy, umbilical hernia and androgen deficiency, on testosterone, presented with non-radiating, moderate to severe right upper quadrant abdominal pain. He reported non-bloody, non-bilious vomiting, but denied melena, hematochezia, jaundice, fever or weight loss. Labs revealed mild polycythemia and elevated AST, ALT levels. CT chest/abdomen/pelvis with IV contrast showed hemorrhagic lesion of the posterior right liver measuring 7.5 cm, favoring hemorrhagic HCA with additional smaller hepatic lesions (Figure 1A). MRI/MRCP abdomen with and without contrast confirmed the findings (Figure 1B). PET scan showed no hypermetabolic uptake within the hepatic adenoma. CEA, CA 19-9 and AFP were normal. Testosterone was stopped, and he got partial resection of the ruptured HCA in segment 6/7. Pathology revealed multifocal HCC within and outside the resected HCA. After discussion at tumor board, he started immunotherapy with Durvalumab. Two months later, repeat MRI abdomen revealed smaller areas of enhancement in segment 4 of the liver. The tumor board advised a biopsy.
Discussion: Malignant transformation is a rare complication of HCAs, with a frequency of 4.2%. Risk factors for malignant transformation include male sex, HCA size > 5 cm, β-catenin activated HCAs, type 1 GSDs, androgen or anabolic steroid intake, and dysplasia in HCAs. Our patient had three risk factors: male, size >5cm and androgen use. This case highlights the two complications that can arise in patients with HCAs: rupture and malignant transformation. It was also peculiar that the malignancy was located inside and outside the HCA. HCAs ≥ 5 cm should be resected given risk of rupture and malignancy. If they are not resected, monitoring with cross-sectional imaging is advised. The absence of malignancy on imaging does not exclude the possibility of malignant transformation. Multidisciplinary discussion is needed for optimal outcomes.
Disclosures:
Emuejevuoke Umukoro, DO1, Kevin Pak, MD2, Julio A. Gutierrez, MD3. P1432 - Hepatocellular Adenoma Presenting With Concomitant Rupture and Hepatocellular Carcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Scripps Mercy Hospital, San Ysidro, CA; 2Naval Medical Center San Diego, San Diego, CA; 3Scripps Clinic, San Diego, CA
Introduction: Hepatocellular adenomas (HCAs) are rare, benign neoplasms from monoclonal proliferation of mature hepatocytes. HCAs mainly occurs in women using oral contraceptive pills (OCPs), but the true population incidence is unknown. It occurs less in men; but the incidence has increased since the 1980s. Though often benign, HCAs can have malignant transformation into hepatocellular carcinoma (HCC). We present a case of a male patient who was found to have a HCA with hepatocellular carcinoma (HCC).
Case Description/Methods: A 44-year-old-male with past medical history of trauma status post left nephrectomy and splenectomy, umbilical hernia and androgen deficiency, on testosterone, presented with non-radiating, moderate to severe right upper quadrant abdominal pain. He reported non-bloody, non-bilious vomiting, but denied melena, hematochezia, jaundice, fever or weight loss. Labs revealed mild polycythemia and elevated AST, ALT levels. CT chest/abdomen/pelvis with IV contrast showed hemorrhagic lesion of the posterior right liver measuring 7.5 cm, favoring hemorrhagic HCA with additional smaller hepatic lesions (Figure 1A). MRI/MRCP abdomen with and without contrast confirmed the findings (Figure 1B). PET scan showed no hypermetabolic uptake within the hepatic adenoma. CEA, CA 19-9 and AFP were normal. Testosterone was stopped, and he got partial resection of the ruptured HCA in segment 6/7. Pathology revealed multifocal HCC within and outside the resected HCA. After discussion at tumor board, he started immunotherapy with Durvalumab. Two months later, repeat MRI abdomen revealed smaller areas of enhancement in segment 4 of the liver. The tumor board advised a biopsy.
Discussion: Malignant transformation is a rare complication of HCAs, with a frequency of 4.2%. Risk factors for malignant transformation include male sex, HCA size > 5 cm, β-catenin activated HCAs, type 1 GSDs, androgen or anabolic steroid intake, and dysplasia in HCAs. Our patient had three risk factors: male, size >5cm and androgen use. This case highlights the two complications that can arise in patients with HCAs: rupture and malignant transformation. It was also peculiar that the malignancy was located inside and outside the HCA. HCAs ≥ 5 cm should be resected given risk of rupture and malignancy. If they are not resected, monitoring with cross-sectional imaging is advised. The absence of malignancy on imaging does not exclude the possibility of malignant transformation. Multidisciplinary discussion is needed for optimal outcomes.
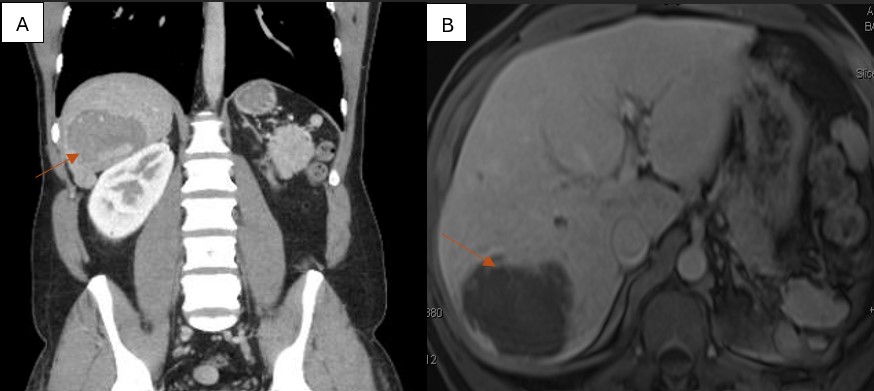
Figure: Figure 1: (A) Coronal view of CT chest/abdomen/pelvis with contrast and (B) Axial view of MRI Abdomen and MRCP with and without Eovist contrast showing 7.5cm hemorrhagic lesion of the posterior right liver, favoring hemorrhagic adenoma.
Disclosures:
Emuejevuoke Umukoro indicated no relevant financial relationships.
Kevin Pak indicated no relevant financial relationships.
Julio Gutierrez indicated no relevant financial relationships.
Emuejevuoke Umukoro, DO1, Kevin Pak, MD2, Julio A. Gutierrez, MD3. P1432 - Hepatocellular Adenoma Presenting With Concomitant Rupture and Hepatocellular Carcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
