Sunday Poster Session
Category: Liver
P1352 - Recurrent Hepatic Encephalopathy in an Adult Without Chronic Liver Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Syed Mujtaba Baqir, MD
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Syed Mujtaba Baqir, MD1, Carla Barberan Parraga, MD2, Jimyeong Son, NP3, Tanuj Chokshi, DO4, James Park, MD5
1Maimonides Medical Center, Brooklyn, NY; 2Maimonides Medical Center, New York, NY; 3Maimonides Medical Center, New Rochelle, NY; 4Maimonides Medical Center, Clifton, NJ; 5Maimonides Medical Center, Manhasset, NY
Introduction: Ornithine transcarbamylase deficiency (OTCD) is the most prevalent inherited disorder of the urea cycle, commonly seen to have an X-linked recessive pattern. It is characterized by inability to metabolize and excrete ammonia leading to an increase in blood ammonia levels and significant neurologic sequele and mortality. Its incidence is known to be between 1 in 56,500 and 1 in 77000. We present a case of ornithine transcarbamylase deficiency, which initially presented as encephalopathy, with a suspicion of liver cirrhosis, however later cirrhosis was ruled out and the presentation was attributed to urea cycle disorder.
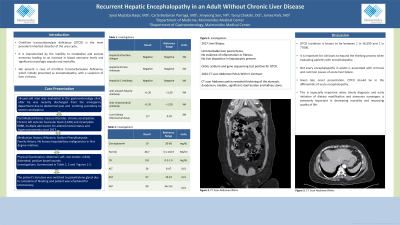
Case Description/Methods: 56-year-old male with past medical history of seizure disorder, chronic constipation, chronic left anterior fascicular block (LAFB) and incomplete RBBB, was evaluated in the gastroenterology clinic after he was recently discharged from the emergency department due to abdominal pain and vomiting secondary to severe constipation. The patient was also noted to have thrombocytopenia and mild elevation of AST. The patient reported that he had multiple admissions for altered mental status secondary to hyperammonemia in 2017. Initially he underwent work-up for liver cirrhosis since his admissions were attributed to hepatic encephalopathy. However, the work-up was negative, including liver biopsy. Following multiple admissions for confusion without a clear precipitant, the patient underwent specific work-up for urea cycle disorder, was found to have orotic aciduria and was diagnosed with Ornithine Transcarbamylase deficiency. The patient was started on lactulose, rifaximin and sodium phenylbutyrate. Following recent discharge from the emergency room, the patient reported bloating and abdominal pain. The patient was advised to continue rifaximin and sodium phenylbutyrate. His lactulose dose was reduced and bisacodyl was added to help with constipation. Due to the chronicity of these symptoms, the patient was scheduled for endoscopy and colonoscopy.
Discussion: It is important for clinicians to expand the thinking process when evaluating patients with encephalopathy. Not every encephalopathy in adults is associated with cirrhosis and common causes of acute liver failure. Given late onset presentation, OTCD should be in the differentials of acute encephalopathy. This is especially important when timely diagnosis and early initiation of dietary modification and ammonia scavengers is extremely important in decreasing mortality and improving quality of life.
Disclosures:
Syed Mujtaba Baqir, MD1, Carla Barberan Parraga, MD2, Jimyeong Son, NP3, Tanuj Chokshi, DO4, James Park, MD5. P1352 - Recurrent Hepatic Encephalopathy in an Adult Without Chronic Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Maimonides Medical Center, New York, NY; 3Maimonides Medical Center, New Rochelle, NY; 4Maimonides Medical Center, Clifton, NJ; 5Maimonides Medical Center, Manhasset, NY
Introduction: Ornithine transcarbamylase deficiency (OTCD) is the most prevalent inherited disorder of the urea cycle, commonly seen to have an X-linked recessive pattern. It is characterized by inability to metabolize and excrete ammonia leading to an increase in blood ammonia levels and significant neurologic sequele and mortality. Its incidence is known to be between 1 in 56,500 and 1 in 77000. We present a case of ornithine transcarbamylase deficiency, which initially presented as encephalopathy, with a suspicion of liver cirrhosis, however later cirrhosis was ruled out and the presentation was attributed to urea cycle disorder.
Case Description/Methods: 56-year-old male with past medical history of seizure disorder, chronic constipation, chronic left anterior fascicular block (LAFB) and incomplete RBBB, was evaluated in the gastroenterology clinic after he was recently discharged from the emergency department due to abdominal pain and vomiting secondary to severe constipation. The patient was also noted to have thrombocytopenia and mild elevation of AST. The patient reported that he had multiple admissions for altered mental status secondary to hyperammonemia in 2017. Initially he underwent work-up for liver cirrhosis since his admissions were attributed to hepatic encephalopathy. However, the work-up was negative, including liver biopsy. Following multiple admissions for confusion without a clear precipitant, the patient underwent specific work-up for urea cycle disorder, was found to have orotic aciduria and was diagnosed with Ornithine Transcarbamylase deficiency. The patient was started on lactulose, rifaximin and sodium phenylbutyrate. Following recent discharge from the emergency room, the patient reported bloating and abdominal pain. The patient was advised to continue rifaximin and sodium phenylbutyrate. His lactulose dose was reduced and bisacodyl was added to help with constipation. Due to the chronicity of these symptoms, the patient was scheduled for endoscopy and colonoscopy.
Discussion: It is important for clinicians to expand the thinking process when evaluating patients with encephalopathy. Not every encephalopathy in adults is associated with cirrhosis and common causes of acute liver failure. Given late onset presentation, OTCD should be in the differentials of acute encephalopathy. This is especially important when timely diagnosis and early initiation of dietary modification and ammonia scavengers is extremely important in decreasing mortality and improving quality of life.
Disclosures:
Syed Mujtaba Baqir indicated no relevant financial relationships.
Carla Barberan Parraga indicated no relevant financial relationships.
Jimyeong Son indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
James Park indicated no relevant financial relationships.
Syed Mujtaba Baqir, MD1, Carla Barberan Parraga, MD2, Jimyeong Son, NP3, Tanuj Chokshi, DO4, James Park, MD5. P1352 - Recurrent Hepatic Encephalopathy in an Adult Without Chronic Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
