Sunday Poster Session
Category: Liver
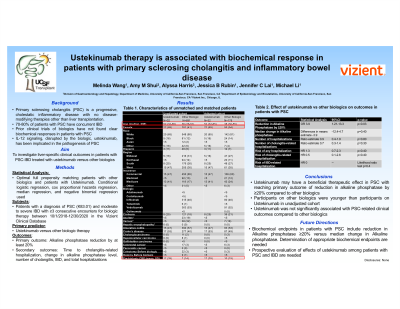
P1230 - Ustekinumab Therapy Is Associated with Biochemical Response in Patients with Primary Sclerosing Cholangitis and Inflammatory Bowel Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Melinda Wang, MD, MHS
University of California San Francisco
San Francisco, CA
Presenting Author(s)
Melinda Wang, MD, MHS1, Amy Shui, MS, MA1, Alyssa Harris, MPH2, Jessica B.. Rubin, MD, MPH3, Jennifer Lai, MD, MBA1, Michael Li, MD, MPH1
1University of California San Francisco, San Francisco, CA; 2Vizient, Inc., Chicago, IL; 3University of California San Francisco and San Francisco VA Health Care System, San Francisco, CA
Introduction: There are currently no therapies proven to slow disease progression in primary sclerosing cholangitis (PSC). About 70% of PSC patients have concomitant inflammatory bowel disease (IBD). While biologics used to treat IBD have not shown any efficacy in PSC to date, ustekinumab suppresses inflammatory signaling by blocking IL-12/23, which may reverse a suppressed regulatory T-cell phenotype associated with PSC. We therefore investigated the effects of ustekinumab on PSC disease activity.
Methods: Adults with a diagnosis of PSC and IBD requiring biologic therapy between 10/1/2018 and 1/1/2021 were included in the study. De-identified data were obtained from the Vizient® Clinical Data Base used by permission of Vizient, Inc. All rights reserved. The data includes patients from >800 US hospital academic, affiliated, and community hospitals. Patients receiving ustekinumab were compared to patients receiving other IBD-related biologics, and propensity score matching was performed utilizing age, sex, and pre-biologic CRP. Logistic regression, Cox regression, median regression, and negative binomial regression were used to identify associations between biologic therapy and PSC outcomes. The primary outcome was reduction in alkaline phosphatase (AP) by at least 20%. Secondary outcomes included cholangitis-related hospitalization, median change in AP, and all-cause hospitalization.
Results: In total, 32 ustekinumab-treated patients were matched with 176 patients treated with other biologics. The median (IQR) age of matched patients was 41 (30-58) years old; 56% were female and 21% had cirrhosis. Patients in the non-ustekinumab group predominantly received infliximab (n=80, 46%) or vedolizumab (n=91, 52%). Ustekinumab-treated patients were more likely to experience a reduction in AP by at least 20% than patients on other biologics (OR 3.9, 95%CI 1.13-13.3, p=0.03). There was no significant difference in time to all-cause hospitalization (HR 1.27, 95%CI 0.69-2.33, p=0.44) or cholangitis-related hospitalization (HR 0.54, 95% CI 0.11-2.62, p=0.45). There also was no significant difference in median change in AP (difference in medians estimate-3.9, 95%CI -12.4 to 4.7, p=0.37).
Discussion: Patients with PSC and IBD treated with ustekinuamb were more likely to experience biochemical response (reduction in alkaline phosphatase by at least 20%) than patients receiving other biologics. Our data suggest that ustekinumab’s potential efficacy in treating PSC should be prospectively investigated.
Disclosures:
Melinda Wang, MD, MHS1, Amy Shui, MS, MA1, Alyssa Harris, MPH2, Jessica B.. Rubin, MD, MPH3, Jennifer Lai, MD, MBA1, Michael Li, MD, MPH1. P1230 - Ustekinumab Therapy Is Associated with Biochemical Response in Patients with Primary Sclerosing Cholangitis and Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California San Francisco, San Francisco, CA; 2Vizient, Inc., Chicago, IL; 3University of California San Francisco and San Francisco VA Health Care System, San Francisco, CA
Introduction: There are currently no therapies proven to slow disease progression in primary sclerosing cholangitis (PSC). About 70% of PSC patients have concomitant inflammatory bowel disease (IBD). While biologics used to treat IBD have not shown any efficacy in PSC to date, ustekinumab suppresses inflammatory signaling by blocking IL-12/23, which may reverse a suppressed regulatory T-cell phenotype associated with PSC. We therefore investigated the effects of ustekinumab on PSC disease activity.
Methods: Adults with a diagnosis of PSC and IBD requiring biologic therapy between 10/1/2018 and 1/1/2021 were included in the study. De-identified data were obtained from the Vizient® Clinical Data Base used by permission of Vizient, Inc. All rights reserved. The data includes patients from >800 US hospital academic, affiliated, and community hospitals. Patients receiving ustekinumab were compared to patients receiving other IBD-related biologics, and propensity score matching was performed utilizing age, sex, and pre-biologic CRP. Logistic regression, Cox regression, median regression, and negative binomial regression were used to identify associations between biologic therapy and PSC outcomes. The primary outcome was reduction in alkaline phosphatase (AP) by at least 20%. Secondary outcomes included cholangitis-related hospitalization, median change in AP, and all-cause hospitalization.
Results: In total, 32 ustekinumab-treated patients were matched with 176 patients treated with other biologics. The median (IQR) age of matched patients was 41 (30-58) years old; 56% were female and 21% had cirrhosis. Patients in the non-ustekinumab group predominantly received infliximab (n=80, 46%) or vedolizumab (n=91, 52%). Ustekinumab-treated patients were more likely to experience a reduction in AP by at least 20% than patients on other biologics (OR 3.9, 95%CI 1.13-13.3, p=0.03). There was no significant difference in time to all-cause hospitalization (HR 1.27, 95%CI 0.69-2.33, p=0.44) or cholangitis-related hospitalization (HR 0.54, 95% CI 0.11-2.62, p=0.45). There also was no significant difference in median change in AP (difference in medians estimate-3.9, 95%CI -12.4 to 4.7, p=0.37).
Discussion: Patients with PSC and IBD treated with ustekinuamb were more likely to experience biochemical response (reduction in alkaline phosphatase by at least 20%) than patients receiving other biologics. Our data suggest that ustekinumab’s potential efficacy in treating PSC should be prospectively investigated.
Disclosures:
Melinda Wang indicated no relevant financial relationships.
Amy Shui indicated no relevant financial relationships.
Alyssa Harris indicated no relevant financial relationships.
Jessica Rubin indicated no relevant financial relationships.
Jennifer Lai: Boehringer Ingelheim – Consultant. Genfit – Consultant. Lipocene – Grant/Research Support. Nestle Nutrition Sciences – Grant/Research Support. Novo Nordisk – Advisory Committee/Board Member. Third Rock Ventures – Consultant. Vir Biotechnologies – Grant/Research Support.
Michael Li indicated no relevant financial relationships.
Melinda Wang, MD, MHS1, Amy Shui, MS, MA1, Alyssa Harris, MPH2, Jessica B.. Rubin, MD, MPH3, Jennifer Lai, MD, MBA1, Michael Li, MD, MPH1. P1230 - Ustekinumab Therapy Is Associated with Biochemical Response in Patients with Primary Sclerosing Cholangitis and Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
